Publications
OPEN examines data, clinical practices and strategies to support better pain management, opioid stewardship, policy, treatment and care.
New Persistent Opioid Use and Associated Risk Factors Following Treatment of Ankle Fractures
Gossett TD, Finney FT, Hu HM, et al. New Persistent Opioid Use and Associated Risk Factors Following Treatment of Ankle Fractures. Foot Ankle Int. 2019;40(9):1043-1051. doi:10.1177/1071100719851117- The rate of new persistent opioid use among patients who underwent one of four open treatments for an ankle fracture was 8.8%, compared with 6.8% among patients who underwent closed treatment.
- New persistent opioid use was not directly linked to injury severity.
- Limiting the peritreatment opioid dose was the largest modifiable risk factor related to new persistent opioid use.
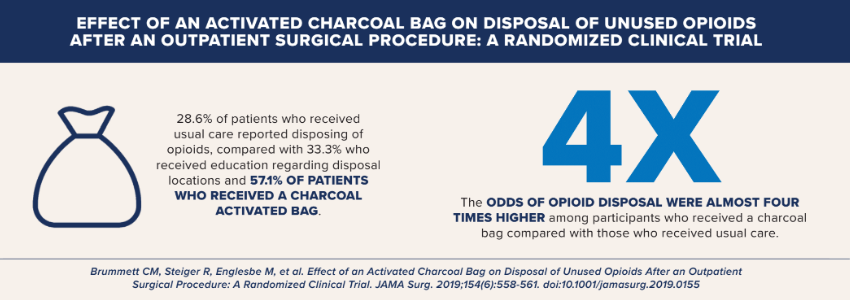
Effect of an Activated Charcoal Bag on Disposal of Unused Opioids After an Outpatient Surgical Procedure: A Randomized Clinical Trial
Brummett CM, Steiger R, Englesbe M, et al. Effect of an Activated Charcoal Bag on Disposal of Unused Opioids After an Outpatient Surgical Procedure: A Randomized Clinical Trial. JAMA Surg. 2019;154(6):558-561. doi:10.1001/jamasurg.2019.0155- 6% of patients who received usual care reported disposing of opioids, compared with 33.3% who received education regarding disposal locations and 57.1% of patients who received a charcoal activated bag.
- The odds of opioid disposal were almost four times higher among participants who received a charcoal bag compared with those who received usual care.
Association Between Long-term Opioid Use in Family Members and Persistent Opioid Use After Surgery Among Adolescents and Young Adults
Harbaugh CM, Lee JS, Chua KP, et al. Association Between Long-term Opioid Use in Family Members and Persistent Opioid Use After Surgery Among Adolescents and Young Adults. JAMA Surg. 2019;154(4):e185838. doi:10.1001/jamasurg.2018.5838- Persistent opioid use occurred in 4.1% of patients with long-term opioid use in a family member compared with 2.4% of patients without long-term opioid use in a family member.
- Long-term opioid use among family members is associated with persistent opioid use among opioid-naïve adolescents and young adults undergoing surgical and dental procedures.
- Physicians should screen young patients for long-term opioid use in their families
Care Coordination for Patients on Chronic Opioid Therapy Following Surgery
Lagisetty P, Bohnert A, Goesling J, et al. Care Coordination for Patients on Chronic Opioid Therapy Following Surgery: A Cohort Study. Ann Surg. 2020;272(2):304-310. doi:10.1097/SLA.0000000000003235- 10% of patients did not have a usual prescriber preoperatively and were more likely to have prescriptions from multiple prescribers and new long-acting opioid prescriptions.
- 8% of patients were exposed to high risk prescribing postoperatively.
- Among patients with a usual prescriber, earlier return was associated with decreased odds of receiving prescriptions from multiple prescribers.
Persistent Opioid Use and High-Risk Prescribing in Body Contouring Patients
Bennett KG, Kelley BP, Vick AD, et al. Persistent Opioid Use and High-Risk Prescribing in Body Contouring Patients. Plast Reconstr Surg. 2019;143(1):87-96. doi:10.1097/PRS.0000000000005084- More than 10% of opioid-naïve patients develop persistent opioid use after body contouring surgery.
- Plastic surgeons must encourage opioid-alternative pain management strategies and optimize transitions of care in vulnerable patients.
Classifying Preoperative Opioid Use for Surgical Care
Vu JV, Cron DC, Lee JS, et al. Classifying Preoperative Opioid Use for Surgical Care. Ann Surg. 2020;271(6):1080-1086. doi:10.1097/SLA.0000000000003109- Preoperative opioid use is common among patients who undergo elective surgery, with 38% filling an opioid prescription in the 12 months before surgery.
- Even minimal opioid use before surgery increases the probability of needing additional postoperative prescriptions in the 30 days after surgery.
- Surgeons should take into account any preoperative opioid use in patients when prescribing and coordinating postoperative pain management.
Spillover Effect of Evidence-Based Postoperative Opioid Prescribing
Howard R, Alameddine M, Klueh M, et al. Spillover Effect of Evidence-Based Postoperative Opioid Prescribing [published correction appears in J Am Coll Surg. 2019 Apr;228(4):720]. J Am Coll Surg. 2018;227(3):374-381. doi:10.1016/j.jamcollsurg.2018.06.007- After introducing evidence-based prescribing recommendations for laparoscopic cholecystectomy, prescribing decreased for four other surgical procedures, with no significant increase in refill requests.
- Implementing evidence-based prescribing recommendations contributes to increased awareness of safe and appropriate opioid prescribing practices.
Association of Opioid Prescribing with Opioid Consumption After Surgery in Michigan
Howard R, Fry B, Gunaseelan V, et al. Association of Opioid Prescribing With Opioid Consumption After Surgery in Michigan. JAMA Surg. 2019;154(1):e184234. doi:10.1001/jamasurg.2018.4234- The quantity of opioid prescribed is associated with higher patient-reported opioid consumption, with patients using .5 more pills for every additional pill prescribed.
- The use of patient-reported opioid consumption to improve prescribing practices is key to combating the opioid epidemic.
Persistent Opioid Use Among Children, Adolescents, and Young Adults After Common Cleft Operations
Bennett KG, Harbaugh CM, Hu HM, et al. Persistent Opioid Use Among Children, Adolescents, and Young Adults After Common Cleft Operations. J Craniofac Surg. 2018;29(7):1697-1701. doi:10.1097/SCS.0000000000004762- 4% of patients who undergo cleft-related surgery continue using opioids following surgery, compared with 0.1% of nonsurgical patients.
- Patients undergoing distractor placement have higher rates of opioid use three months after surgery.
- New persistent opioid use occurs after cleft-related procedures and can lead to chronic use in children, adolescents, and young adults.
A Statewide Comparison of Opioid Prescribing in Teaching Versus Nonteaching Hospitals
Cron DC, Hwang C, Hu HM, et al. A statewide comparison of opioid prescribing in teaching versus nonteaching hospitals. Surgery. 2019;165(4):825-831. doi:10.1016/j.surg.2018.10.005- In Michigan, surgical patients discharged from teaching hospitals fill significantly larger opioid prescriptions and have higher rates of high-risk prescribing compared with patients discharged from nonteaching hospitals.
- All hospitals, particularly teaching hospitals, should devote adequate resources to facilitating safe postoperative opioid prescribing.


