Open  Healthcare Professionals
Healthcare Professionals
We offer evidence-based best practices and the latest research in an effort to support healthcare professionals and change the trajectory of the opioid epidemic. On this site, you’ll find up-to-date resources for: 
Adult Prescribing Recommendations
Use OPEN’s evidence-based prescribing recommendations for tailored pain management after surgery in adult patients.

Pediatric Prescribing Recommendations
Use OPEN’s Pediatric evidence-based acute care opioid prescribing recommendations after surgery.
Pediatric Surgical Pain Management Toolkit
Learn about prevention of opioid-related complications in children and adolescents after surgery.
Acetaminophen and NSAIDs Reference Sheet – Dentistry
Learn more about prescribing acetaminophen and NSAIDs for pain management after dental surgery.

Surgical Prescribing: Summary of Best Practices
Stay up to date with OPEN’s summary of best practices for prescribing after surgery.

Educational Webinars YouTube Playlist
Missed a webinar or want to go back and rewatch one? Visit our YouTube playlist to find our past webinars.
Fentanyl Test Strips Step-by-Step Instructions
Learn how to use fentanyl test strips to reduce risk of an overdose.

Fentanyl Test Strip Pocket Guide
Learn how to use fentanyl test strips to reduce risk of an overdose.
Managing Pain After Childbirth Toolkit
A practical guide for clinicians to learn more about implementing the COMFORT (Creating Optimal Pain Management for Tailoring Interventions after Childbirth) Clinical Practice Guideline.

Opioid Use in Michigan (2019): A Review of County-Level Opioid and Poverty-Related Data
Utilize our new Landscape Map and accompanying whitepaper to help reduce the impact of the opioid crisis.

Managing Pain After Childbirth
Learn ways to manage pain after childbirth such as: over-the-counter medications, non-medication strategies, and opioids, if prescribed.
Adult Surgery Pain Management Guide for Patients
Learn how to prepare for surgery and to help manage pain after surgery.

Adult Surgery Pain Management Guide for Healthcare Providers
As a healthcare provider, learn evidence-based approaches to help manage your patient’s pain after surgery.
Dental Prescribing: Summary of Best Practices
Stay up to date with OPEN’s summary of best practices for prescribing after dental surgery.
Take A.C.T.I.O.N. Naloxone Training
Take our Naloxone Training and learn how to take A.C.T.I.O.N to reverse an overdose.

Managing Pain After Dental Surgery
Learn ways to manage pain after dental surgery such as: over-the-counter medications, non-medication strategies, and opioids, if prescribed.
Managing Pain After Surgery (Adults)
Learn ways to manage pain after surgery such as: over-the-counter medications, non-medication strategies, and opioids, if prescribed.

Non-Medication Pain Management
Learn how to help manage or reduce your pain and anxiety through various techniques.

Pediatrics Non-Medication Pain Management
Learn how to help manage your child’s pain and anxiety after surgery.

4 Evidence-based Reasons To Improve Opioid Prescribing Practices After Surgery
Explore 4 evidence-based reasons to improve opioid prescribing practices after surgery.

4 Evidence-based Reasons To Improve Opioid Prescribing Practices After Dental Surgery
Explore 4 evidence-based reasons to improve opioid prescribing practices after dental surgery.

Sharps and Liquids Safe Disposal
Learn how to safely dispose of needles, lancets, and liquid medications.

Transitional Pain Service Financial Tool
Explore our free financial tool to tailor insights to your organization on the potential costs and benefits of starting a transitional pain service.
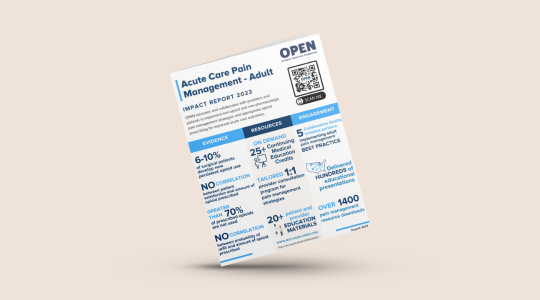
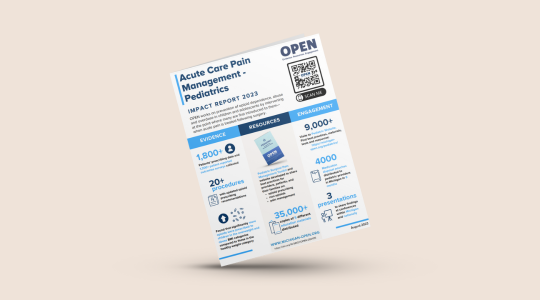
Acute Care Pain Management – Adult Impact Report
Learn about OPEN’s impact with acute care pain management.

Opioid Prescribing Recommendations Impact Report
Learn about OPEN’s impact with our opioid prescribing recommendations.
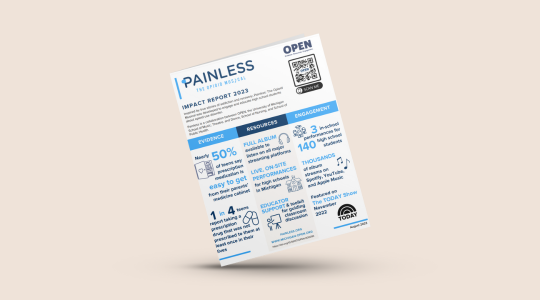
Painless: The Opioid Musical Impact Report
Learn about the impact that Painless: The Opioid Musical has had in our communities.
Managing Addiction Stigma in Treating Pain and OUD
This video details ways to manage addiction stigma while treating pain and OUD.
Ending Addiction Stigma
This video will explain the importance of ending addiction stigma and fully supporting OUD patients.

Painless: The Opioid Musical Lyrics Sheet
Use these lyrics to follow along with Painless and reference them for discussion about the stories that are told in the musical.

Painless: The Opioid Musical Toolkit
Equip educators with everything they need to effectively bring Painless: The Opioid Musical to life.
Pain and Opioid Data Collection
Explore OPEN’s process to create and evaluate opioid prescribing recommendations.

Law Enforcement Officers Roundtable Discussion
Learn from Law Enforcement Officers as they discuss SUD and OUD.
Intranasal Naloxone for First Responders Instructional Video
Teach first responders how to use intranasal naloxone.
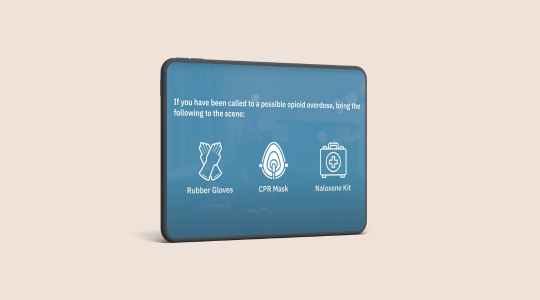
First Responder Overdose Response – Take ACTION
Equip first responders on how to handle an opioid overdose with naloxone.

Levels of Evidence
Explore the five Levels of evidence to use while making educated determinations about prescribing and care.
Perioperative Pain Management and Care Coordination for Surgeons CE Course
This free, 3-hour CE course will empower surgical providers to directly impact the opioid epidemic by learning best-practice care strategies.
Perioperative Pain Management and Care Coordination for Primary Care Providers CE Course
This free, 3-hour CE course will empower primary care providers to directly impact the opioid epidemic by learning best-practice care strategies.
Pain Management in Dentistry CE Course
This free, 3-hour CE course will empower dental providers to directly impact the opioid epidemic by learning best-practice care strategies.

Pediatric Planning For Surgery and Pain Management Worksheet
Use and share this worksheet with your child’s care team to help prepare and manage pain after your child’s surgery.

Opioid Prescribing for Wisdom Tooth Extraction
Check out this one-minute video about non-opioid pain management options for children and teens after wisdom teeth removal. Video captions are in Arabic.

Permanent Disposal Guide
Learn how to implement a permanent medication disposal box program in your community.

Words Matter Video – Shatterproof
Changing our language improves outcomes for those struggling with addiction. Watch this brief video to learn more.
Addiction Language Guide – Shatterproof
Comprehensive addiction language guide to reduce use of stigmatizing language.
Substance Use Disorder Screening and Care Coordination Toolkit
Use these customizable email templates to communicate best care practices for patients with positive TAPS screening category.

Medication Disposal
Learn how to facilitate discussion on safe disposal of unused opioids with your healthcare provider.
Acetaminophen and NSAIDs Reference Sheet – Surgery
Learn more about prescribing acetaminophen and NSAIDs for pain management after surgery.

Guideline for Prescribing Opioids for Chronic Pain (CDC)
Intended to improve communication between providers and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder and overdose.

Impacting the Opioid Crisis: Prevention, Education, and Practice for Non-Prescribing Providers
This free, 16-hour CE course will empower non-prescribing providers to directly impact the opioid epidemic through increased knowledge and tools to transform practice and policies.

How to Perform Rescue Breathing – Take ACTION Overdose Training
Learning to perform rescue breathing on someone who is experiencing an opioid overdose.
Intranasal Naloxone for Laypeople – Take ACTION Training
Learn to use intranasal naloxone to reverse an opioid overdose.
Naloxone Community Layperson Training – Take ACTION Training
Naloxone training for community laypeople.

Michigan Opioid Collaborative – Addressing OUD Stigma Presentation
Emily McCall and Tim Shewcraft from the Michigan Opioid Collaborative (MOC) share information about stigma and MOC’s resources for MOUD providers. Tim, a peer recovery coach, shares his personal experience with stigma and the impacts that provider stigma can have on a patient’s OUD treatment.
Emergency Department Naloxone Implementation Guide
Learn how to facilitate and implement unique and tailored naloxone distribution programs in your Emergency Department.

How Do You Treat Pain? (For Teens)
A one-page flyer created by the Pediatric Trauma Group at C.S. Mott Children’s Hospital focused on non-medication options for teens.

Non-Drug Options for Pain Management and Comfort in Children
A document created by Michigan Medicine Child Life providing greater detail on non-medication strategies.
Medication Tracking Log
Help keep track of the use of medications your child is taking after surgery.

Medication Take Back Event Guide
Learn how to successfully host a Medication Take Back Event in your community.

COVID’s Impact on the Opioid Crisis
This video will discuss the impact of COVID-19 on the opioid crisis.

COVID’s Impact on the Treatment of Opioid Use Disorder
This video will discuss the impact COVID-19 had on the treatment of Opioid Use Disorder.