Explore our free financial tool to tailor insights to your organization on the potential costs and benefits of starting a transitional pain service.

What is a transitional pain service (TPS)? A TPS is a program that aims to identify and manage patients who are at high risk for poor pain outcomes after surgery. Many of these patients have chronic pain, are on long-term opioid treatment, and/or have a history of addiction. The service optimizes the pain regimen of these patients before their surgery, manages them during the post-surgical inpatient stay (if applicable), and provides follow-up care in the outpatient setting once they leave the hospital.
How can a TPS be beneficial to patients and hospitals? Approximately five to ten percent of patients undergoing surgery are considered high risk for poor pain-related and opiate-related outcomes. Patients with high pain levels after surgery use more healthcare resources than their non-high-risk counterparts, as they experience longer hospital stays, higher readmission rates, more Emergency Department visits, and more surgery clinic visits. Institutions around the U.S. and in Canada have demonstrated that a TPS may be beneficial for reducing pain levels and opioid doses after surgery as well as healthcare utilization.
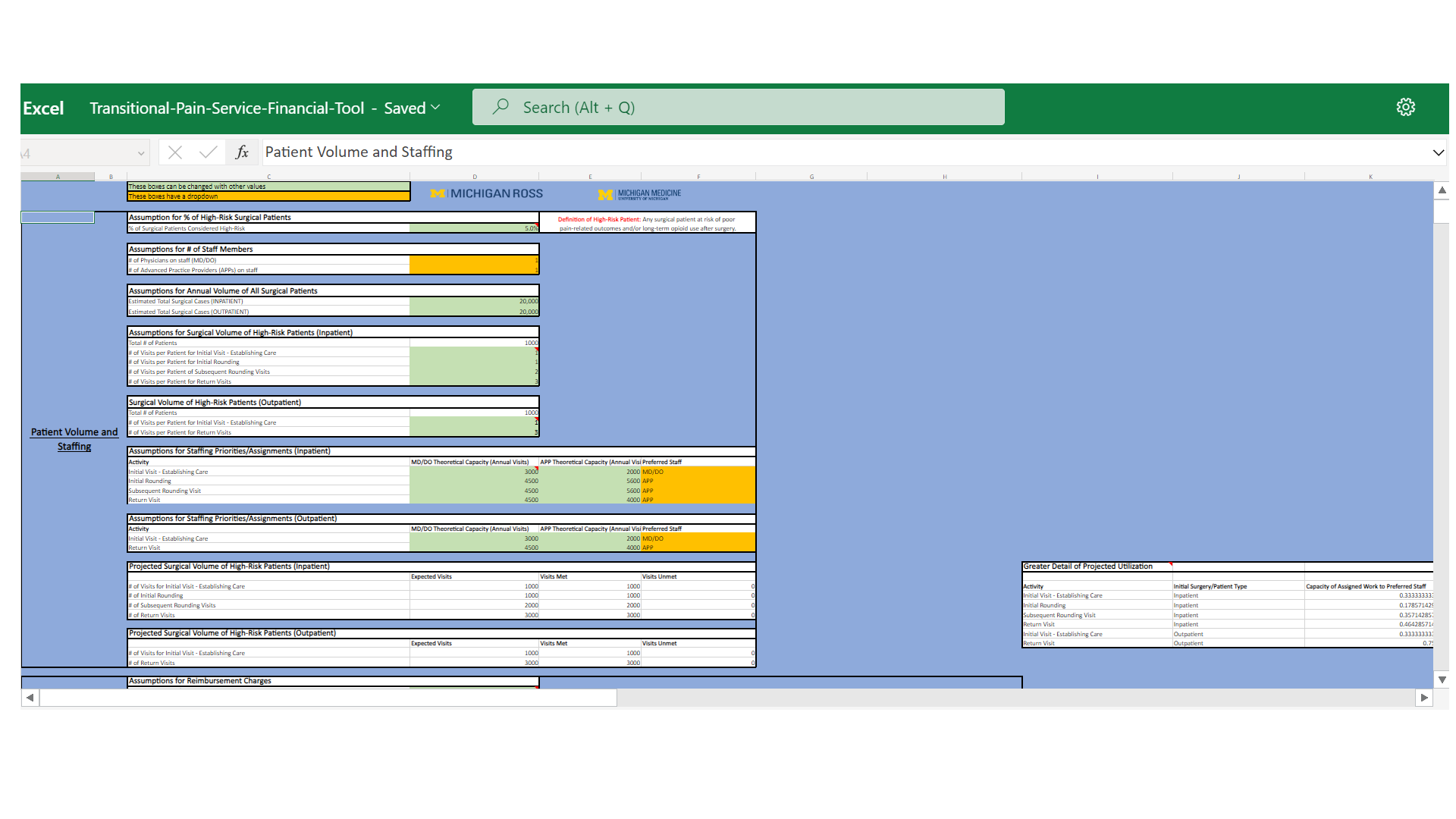
How can a financial tool help? Our hope is that this financial tool can offer healthcare institutions a prediction into the costs and financial returns from implementing a TPS. It may also assist in guiding institutions to make financially sound decisions based on the possible staffing models specific to their organization.
About the financial tool: The authors developed this modifiable financial modeling tool, which can be tailored to any healthcare institution. Inputs include details related to staffing, total surgical volumes, inpatient and outpatient volumes, staffing capacity, and revenues generated by each staff member. Indirect cost savings are calculated from predicted changes in length of stay, emergency department visits from post-surgical pain, and revenue opportunity due to open beds from reducing length of stay.
Financial insights from this model are predictions based on various estimates and assumptions. OPEN is not liable for institutional decisions and outcomes guided by this tool.
References:
Clarke, H. (2016). Transitional pain medicine: Novel pharmacological treatments for the management of moderate to severe postsurgical pain. Expert Review of Clinical Pharmacology, 9(3), 345–349. https://doi.org/10.1586/17512433.2016.1129896
Haroutiunian, S., Nikolajsen, L., Finnerup, N. B., & Jensen, T. S. (2013). The neuropathic component in persistent postsurgical pain: A systematic literature review. Pain, 154(1), 95–102. https://doi.org/10.1016/j.pain.2012.09.010
Lee, J. S., Vu, J. V., Edelman, A. L., Gunaseelan, V., Brummett, C. M., Englesbe, M. J., & Waljee, J. F. (2019). Health care spending and new persistent opioid use after surgery. Annals of Surgery, 272(1), 99–104. https://doi.org/10.1097/sla.0000000000003399
McAnally, H. (2017). Rationale for and approach to preoperative opioid weaning: A preoperative optimization protocol. Perioperative Medicine, 6(1). https://doi.org/10.1186/s13741-017-0079-y
Mikhaeil, J., Ayoo, K., Clarke, H., Wąsowicz, M., & Huang, A. (2020). Review of the transitional pain service as a method of postoperative opioid weaning and a service aimed at minimizing the risk of chronic post-surgical pain. Anaesthesiology Intensive Therapy, 52(2), 148–153. https://doi.org/10.5114/ait.2020.96018
Shechter, R., Speed, T. J., Blume, E., Singh, S., Williams, K., Koch, C. G., & Hanna, M. N. (2019). Addressing the opioid crisis one surgical patient at a time: Outcomes of a novel Perioperative Pain Program. American Journal of Medical Quality, 35(1), 5–15. https://doi.org/10.1177/1062860619851170