In the past, there has been an excess of opioid prescribing after dental surgeries like wisdom tooth extraction, leading to increased risks of opioid use disorder. OPEN has compiled years of research into tools to help providers have access to the best prescribing practices. OPEN strives to give patients and providers the tools they need for pain management by promoting the use of non-opioid and non-medication pain management strategies for improved patient outcomes.

OPEN strives to give patients and providers the tools they need for pain management. Learn about preparing for dental procedures, talking with your dentist, and strategies to manage pain such as over-the-counter medications, non-medication options, and opioid medications.
Pain after certain dental procedures is normal and expected. You may hear it called acute pain, because, while it can cause considerable discomfort, it usually begins to get better a few days after the procedure. Before the procedure, talk with your dentist about any medications or substances you take as these may impact your pain control. Ask your dentist what type of pain is expected after the procedure and what you should do to control your pain. Options to control pain may include using over the counter (OTC) medications, non-medication options and if prescribed, opioid medications. If you are prescribed an opioid medication, it is important to know the risks, potential dangers and side effects, and how to minimize risk to yourself and others.
Each person recovers from procedures in their own way, and someone who has the same procedure might have a completely different experience of pain. Pain after procedures is normal and tells you that your body is healing, and you might need to balance activity with rest. It is an uncomfortable but natural part of recovery. While everyone feels pain differently, typically procedural pain is the worst during the first 2-3 days after and then begins to get better.
The goal of pain management is for you to do activities of daily living like:
Pain may be well-controlled with a schedule of over the counter (OTC) medications like acetaminophen (Tylenol®) and ibuprofen (Motrin®, Advil®). Adding non-medication options to your pain management plan can help to successfully treat pain.

Learn ways to manage pain after dental surgery such as: over-the-counter medications, non-medication strategies, and opioids, if prescribed.
Ask your surgeon about:
| Mindfulness or Meditation | Music | Books |
| Calm breathing, like belly breathing or square breathing, can help to relax muscles that are tense because of pain or anxiety. This is called Mindful Breathing. You can also focus your mind and visualize a particular place you enjoy that makes you feel calm, relaxed, and comfortable. | Music may be very comforting when you are experiencing pain or discomfort. Listening to music, singing, or writing songs can help to lessen pain and anxiety. | Before surgery, take time to select a few books that you would like to read while you are recovering. This can help you to feel relaxed and distraction from pain after surgery. |
| Sleep or Relaxation | Ice or Heat | Compression |
| Take time during your recovery to rest and relax. Sleep helps the body heal. | Talk to your surgeon to determine if ice or heat would be helpful to your recovery. | Talk to your surgeon to determine if compression of the surgery area would be helpful to your recovery. Using an ‘abdominal binder’ after surgery can provide comfort especially when moving around. |
| Short walks | ||
| Taking a short walks after surgery is so important! Walking helps to: -Get blood flowing in your body which helps you heal and reduces risk of developing blood clots -Regain your strength and mobility before surgery -Reduce constipation -Improve mood and anxiety |
Using medications like ibuprofen (Motrin or Advil) and acetaminophen (Tylenol), that you can purchase at your local pharmacy, can be very effective at managing your pain after surgery. Each works in different ways to manage pain and can be taken together at the same time.
Ask your surgeon:
Sample schedule and doses for OTC medications:
| Time | Medication (Dose) |
|---|---|
| 9 AM | TYLENOL (1000mg) MOTRIN (600mg) |
| 3 PM | TYLENOL (1000mg) MOTRIN (600mg) |
| 9 PM | TYLENOL (1000mg) MOTRIN (600mg) |
Dental providers can find current evidence to support appropriate opioid prescribing, best practices for pain management, opioid prescribing recommendations which can be tailored to meet patient needs, counseling suggestions to educate patients on postoperative expectations, and care coordination strategies to manage complex care needs.

Explore 4 evidence-based reasons to improve opioid prescribing practices after dental surgery.
Our research examined opioid use among those exposed to opioids for the first time after wisdom tooth extraction. In a study of nearly 71,000 people ages 13–30 not using opioids** before undergoing wisdom tooth extraction:
People exposed to opioids for the first time after other elective surgeries are at an increased risk for persistent opioid use. Opioid prescribing after wisdom tooth extraction is linked to persistent opioid use*.
*For this study, persistent opioid use was defined as one or more opioid prescription fills during days 4–90 after the procedure, in addition to one or more fills during days 91–365, written by any provider for any reason.
**For this study, this was defined as no opioid prescriptions filled in the 6 months prior to the procedure.
This free, 3-hour CE course will empower dental providers to directly impact the opioid epidemic by learning best-practice care strategies.
People exposed to opioids for the first time after other elective surgeries are at an increased risk for persistent opioid use. Research at Michigan OPEN examined opioid use among those exposed to opioids for the first time after wisdom tooth extraction.
Since acetaminophen and ibuprofen are available over the counter and don’t require a prescription for patients to use, patients and their caregivers often do not receive instructions on how to use them after surgery. The packaging instructions for acetaminophen and ibuprofen provide minimal dosing and recommend as-needed use. If these instructions are followed, patients may be underdosed and inadequately addressing their pain. In addition, if patients were prescribed an opioid, they may think this is the first medication they should use for their pain, not understanding that acetaminophen and ibuprofen often provide adequate pain relief when appropriately dosed and that an opioid may not be needed. *Unless contraindicated
For more information about prescribing and dosing Acetaminophen and NSAIDs, see OPEN’s Surgical Pain Management Initiative.

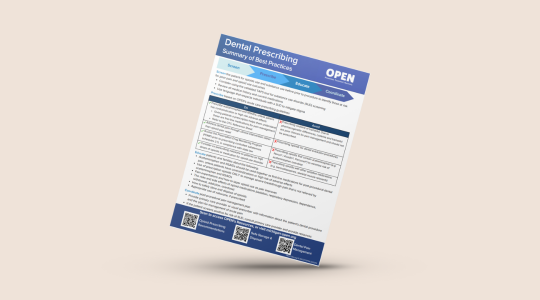
Stay up to date with OPEN’s summary of best practices for prescribing after dental surgery.
Screen for opioid use and substance use before surgery to identify those at risk for poor pain and opioid use outcomes
Educate patients and families:

Explore 4 evidence-based reasons to improve opioid prescribing practices after dental surgery.

Learn ways to manage pain after dental surgery such as: over-the-counter medications, non-medication strategies, and opioids, if prescribed.

Check out this one-minute video about non-opioid pain management options for children and teens after wisdom teeth removal. Video captions are in Arabic.

Learn how to help manage or reduce your pain and anxiety through various techniques.