OPEN is working to reduce opioid-related deaths by expanding access to naloxone among high-risk populations. Our strategy is to collaborate with organizations and institutions across Michigan to distribute naloxone and get this life saving medication into the hands of patients, family members, caregivers and communities who are at high risk of opioid overdose.

| Intramuscular | Nasal Spray (Narcan) | |
|---|---|---|
| Appearance |  |  |
| Duration of Action | 30-90 minutes | 20-120 minutes |
| Repeat Dosing | Every 2-3 minutes | Every 2-3 minutes |
| Strength | 0.4mg/mL | 4mg |
| Assembly Supplies Needed | #2, 3 mL syringe w/ 23-25 gauge 1-1.5 inch IM needles | None |
| SIG for Suspected Overdose | Inject 0.4 mg (1 mL) IM x1. Repeat every 2-3 minutes until patient is responsive or EMS arrives | 1 actuation in one nostril x2. Repeat every 2-3 minutes until patient is responsive or EMS arrives |
| Storage | -Protect from light -Room temperature - 68 °F to 77 °F | -Protect from light -Room temperature - 68 °F to 77 °F -Excursion allowed between 41 °F and 104 °F -Freezes at temperatures below 5 °F and the device will not spray. Leave the device at room temperature for 15 minutes to thaw |
| How is it Supplied | Single dose flip top vial | Carton contains 2 blister packages of 4mg single use nasal spray |
| Disposal | Sharps container | Any waste container that is away from children |
| Direct Cost | $30-40 | $169 |
Michigan law protects you from liability when giving naloxone and calling 911 for someone who is experiencing an overdose.
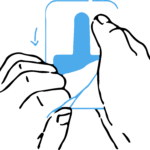 | 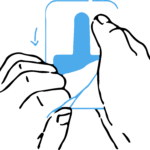 |  |
| Step 1: Peel from packaging. | Step 2: Place the nozzle in the nose. | Step 3: Push the plunger to spray. |
OPEN offers free, online and self-paced training to learn how to help someone experiencing an overdose.
First responders are key players in responding to our country’s opioid overdose epidemic. Take our First Responder Training to learn how to reverse an overdose.
Allies, community leaders, and those wanting to impact and save lives: take our Community Layperson Naloxone Training and learn how to take A.C.T.I.O.N to reverse an overdose.
When someone is experiencing an overdose, every second matters. Knowing what to do—and quickly—can help save a life and give a person another opportunity for recovery.
 | A | Arouse (3 S's) |
|
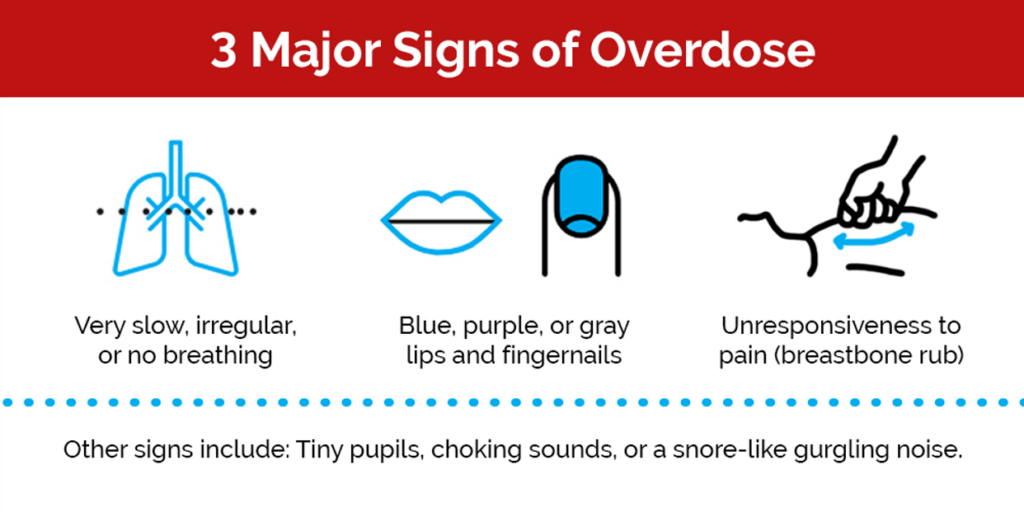
 | C | Check for signs of overdose |
|
 | T | Telephone 911 |
|
 | I | Intranasal Naloxone |
|
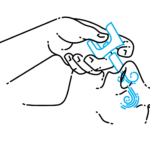
 | O | Oxygen |
|
 | N | Naloxone again |
|
The pharmacies below have a standing order for naloxone. Pharmacists can dispense naloxone for a fee. Select your county below to see a specialized, shareable brochure on where to find naloxone near you:
Prescribing naloxone to patients in the emergency department (ED) setting is recommended, legal, and within the scope of practice, carrying no more liability than the prescribing of other medications. ED-based naloxone distribution is impactful and cost effective. Organizations face several obstacles when establishing a program, including educating and training staff and lack of resources required to effectively introduce and sustain these evidence-based practices. This detailed guide is designed to facilitate implementation of your unique ED tailored naloxone distribution program.

Learn how to facilitate and implement unique and tailored naloxone distribution programs in your Emergency Department.
It is important to develop a team of members familiar with all the different aspects of building an ED naloxone program. Your team members can provide process improvement expertise and serve as champions for the work, advocating for naloxone distribution as a critical harm reduction intervention.
Currently, no validated screening tools exist for acute care settings. The CDC and other studies have recommendations for identifying patients at higher risk for overdoses (see Box 2). Your team should decide which patient population will be targeted to receive naloxone rescue kits.
EHR prompts are associated with increased naloxone distribution for patients after overdoses. Work with your IT department to build order sets and alerts to facilitate the process.
By teaching your multidisciplinary team how to educate patients, anyone can address patient questions or concerns.
Consider the patient’s health literacy level as well as any reading or comprehension issues.
OPEN offers several free patient education resources (link or jump to resources section?).
Ideal Standard:
OPEN partners with MEDIC to increase access to naloxone by supplying emergency departments with take-home naloxone kits. Learn more about our partnership.

Learn how to facilitate and implement unique and tailored naloxone distribution programs in your Emergency Department.