Medication for opioid use disorder (MOUD) is the gold standard evidence-based treatment for opioid use disorder (OUD). There are several things to consider when using MOUD, including: type of medication to start such as buprenorphine, initiation dosing methods, frequency of follow-up visits, potential withdrawal support, treatment maintenance, urine drug screening, and potential return to use. Explore frequently asked questions to learn more.

Medication for opioid use disorder (MOUD) is the gold standard evidence-based treatment for opioid use disorder (OUD). There are three FDA-approved medications for OUD: methadone, buprenorphine, and naltrexone. These medications are essential in the treatment and management of addiction to opioids. Notably, methadone and buprenorphine are the only treatments for OUD associated with up to 50% reduction in opioid overdose and death.1 MOUD treatment has been proven to effective in2:

Buprenorphine is a partial opioid agonist that binds to the mu-opioid receptors in the brain but activates the receptors to a lesser extent than full opioid agonists such as heroin or methadone. This partial activation provides analgesia and relief from withdrawal symptoms and cravings without the full respiratory depressive effects seen with full agonists. This helps protect against overdose. Buprenorphine binds very tightly to opioid receptors, which makes it effective in blocking other opioids. Buprenorphine stabilizes the receptors in the brain and decreases disruption of the pleasure reward pathways. Buprenorphine is available in various forms including long acting injectables and is often combined with naloxone to further deter misuse and diversion.
Buprenorphine Formulations3
Approved for OUD:
Other formulations approved for pain:
Extended-release, injectable naltrexone (Vivitrol) is an (FDA) approved opioid antagonist used to treat OUD. It is also available in pill form but that is not approved for OUD. It is not a controlled substance. Naltrexone blocks the effects of opioids, preventing intoxication and physical dependence. This reduces the rewarding aspects of opioid use that create cravings for more. Naltrexone can be prescribed and administered by any clinician with a license to prescribe medications and is administered monthly by a clinician. Naltrexone does not help acute opioid detoxification and withdrawal symptoms. An individual must complete detoxification and withdrawal from opioids before starting Naltrexone to avoid precipitated withdrawal.
Naltrexone Formulations3

Methadone is a schedule II-controlled medication and is a long-acting full opioid agonist. It reduces cravings and withdrawal symptoms by acting on opioid receptors in the brain. Methadone can only be dispensed through a SAMHSA certified Opioid Treatment Program (OTP). Methadone is the most studied pharmacotherapy for OUD and has by far the longest track record (nearly 50 years).
Methadone Formulations3
Buprenorphine diversion is often associated with avoiding withdrawal symptoms and other opioid use or helping someone else avoid withdrawal symptoms. Here a few points in addressing and responding to suspected diversion:
The information below is meant to be used as a general guide when completing an assessment for substance use. For tools, algorithms, and documentation tips, visit: OBAT Clinical Tools and Forms | Resources | Grayken Center for Addiction TTA | Boston Medical Center.
| Substance | Age of first use | Date of last use | Quantity | How often | Route | Treatment history | Periods of sustained abstinence | Consequences of use |
|---|---|---|---|---|---|---|---|---|
| Oxycodone | 15 | 6/10/24 | 10 tablets | Daily | Snort | Residential in 2022 | 3 months in 2022 | Lost job |
Once the provider and patient decide together to move forward with starting buprenorphine consider the following steps.

Use this sample agreement as a starting point when prescribing buprenorphine.
 service!
service!In general, there are three methods for initiating buprenorphine, but strategies for initiation in practice can vary greatly based on clinician and patient. Standard and low dose initiation are safe and effective as home-based initiation. A third strategy, high dose initiation, is being explored but currently not used widely in the outpatient setting. All strategies are most effective with check-ins from a clinical staff member during the initiation process. Evidence shows that a higher initiation dose of buprenorphine (at least 16 mg) is associated with decreased return to opioid use and better retention in treatment, particularly for patients using fentanyl (thus with high tolerance).
General Considerations:
This strategy requires the patient to be in opioid withdrawal. The patient stops their full opioid for approximately 12-72 hours (depending on type of opioid used), experiences withdrawal symptoms, and then begins buprenorphine. Withdrawal support medications can aid in this process.

This document is a guideline to starting buprenorphine at a standard dose.
This strategy requires that the patient continues their full agonist while increasing buprenorphine. The patient initiates a very low dose of buprenorphine (typically starting at 0.5mg), slowly increasing the dose daily over a period of time while continuing to use their full opioid agonist at their usual dose. Continuation of the full opioid agonist is vital to success with this strategy. Only after the period of initiation is over (typically 7 days, though 3 day protocols are also used at times) does the patient stop their full opioid agonist. When carried out correctly, the patient should never experience any withdrawal symptoms.
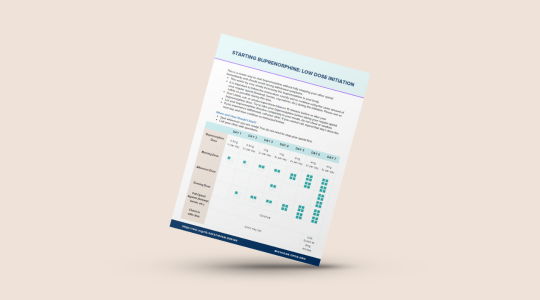
This document offers a guideline to starting buprenorphine at a low dose.
This initiation strategy originally started in emergency departments after a patient had an overdose and was given Naloxone. It requires that the patient stop their opioid agonist for approximately 8-48 hours and experiences withdrawal. In contrast to the traditional initiation, dosing escalates rapidly on the first day to reach 24-32 mg buprenorphine.
The below examples are brief, simplified cases for educational purposes and are not meant to be advice for a particular patient case. Shared decision-making with the patient is key to success.
Always offer opioid withdrawal support medications, for any type of initiation. If pursuing traditional or high dose initiation, encourage patients to start withdrawal support medications prior to their most significant withdrawal symptoms. Discuss with patients which medications are helpful for which symptom. These medications can be helpful to start a few hours after last use and prior to onset of withdrawal symptoms:
*Off-label use.

This resource will help providers successfully provide withdrawal comfort and support.
Stabilizing a patient on buprenorphine involves transitioning the patient from a state of opioid dependence or addiction to a stable state where cravings and withdrawal symptoms are effectively managed. Once stabilized on OUD medication, many patients stop using illicit opioids completely. Others continue to use for some time, but less frequently and in smaller amounts, which reduces their risk of morbidity and overdose death.
Schedule regular appointments to monitor the patient’s progress, adherence, and any side effects. Determining the patient’s follow up schedule should be done through good clinical judgment and shared decision making with the patient. According to the Boston Medical Center Office Based Addiction Treatment manual, “Once stable, clinic visits can be every 2 to 4 weeks with refills that coincide with visits.” Initially, visits may be weekly for the first month and then gradually increase the time in between as the patient makes progress. During these visits, talk to the patient about how they are doing and make adjustments to ensure the dose of medication is effective and tailored based on withdrawal symptoms, cravings, side effects, current substance use, social supports, etc.5

Although research on the optimal duration of addiction treatment is limited, existing studies generally indicate that longer treatment periods lead to better outcomes according to the American Society of Addiction Medicine’s 2020 Clinical Guidelines.2 Similarly, SAMHSA’s TIP 63 Medications for Opioid Use Disorders (2021) states that the most favorable results are achieved when patients continue to receive medication for as long as it remains beneficial, a strategy often referred to as “maintenance treatment.”5 Studies suggest rates of 50-90% of patients return to opioid use at least one month after buprenorphine taper/discontinuation. Evidence supports better outcomes with longer retention in treatment.
If a patient expresses a desire to discontinue treatment, talk to them about things such as:
People with substance use disorder experience incidents of relapse just like others do with chronic diseases like diabetes, hypertension, and asthma.6

Using medication to treat opioid use disorder, combined with supportive counseling and therapy that addresses both the physical and psychological aspects of addiction, produces the best remission outcomes. Precipitants to return to use often include negative affect, response to stressors and stimuli, or family/relational conflict. Cravings/cues like people, places, things, social pressures, and stress can precipitate a return to use.
If a patient has returned to use, do NOT discharge them from your care but rather attempt to re-engage with the patient. Use this as an opportunity to re-evaluate a patient’s care plan, explore other opportunities, and determine if a higher level of care may be appropriate just as we do for other chronic diseases.

“Providers should order the right test, for the right patient, at the right time, with the goal of conducting toxicology screening only as often as needed to create an appropriate treatment plan that supports patient safety and recovery goals.”5 Urine drug screening (UDS) practices should focus on supporting patient wellness and recovery, not surveillance or punishment, and drug screening results should never be the sole basis for a treatment decision. It is important to recognize that because UDS is used in many different settings including legal and carceral settings, patients may be apprehensive about UDS due to the historical punitive nature of these contexts. Patients should always be informed that a UDS is ordered and never done blindly without a patient’s knowledge.
Offers more information about testing and interpretations along with treatment implications.5
Massachusetts Nurse Care Manager Model of Office Based Addiction Treatment: Clinical Guidelines.4

Use this guide to help order urine testing and interpret the results.
Below is a list of frequently asked questions from our Medication for Opioid Use Disorder Trainings. Interested in attending a training? Check out our events page!

When taken correctly, naloxone won’t be active, so both medications theoretically should have the same therapeutic effect.
The buprenorphine/naloxone (Suboxone®) is considered an abuse deterrent formulation. If taken as prescribed (sublingual) the only buprenorphine works as expected, however if it is injected, the antagonist (naloxone) blocks the effect of the buprenorphine.
Injectable formulations are very effective for some patients. There are two different long-acting buprenorphine injectable formulations- Brixadi® and Sublocade®. For some patients with a very high tolerance, the step-down dose of Sublocade® is not enough. In these cases, we may continue the 300 mg dose, but can be very effective and can break some of the behavioral aspects of self-managing medications. Suboxone® also has a long half-life so as long as they take it daily, they reach a very stable steady state.
It is uncommon to “need” the non-abuse deterrent form (buprenorphine alone, rather than Suboxone®). It used to be recommended for pregnant patients but now Suboxone® is used in all situations.
Buprenorphine/naloxone (Suboxone®) is an opioid so when people are physically dependent on any opioid if they stop they will go through withdrawal.
There is no difference in rate of precipitated withdrawal with buprenorphine (Subutex®) and buprenorphine/naloxone (Suboxone®). The buprenorphine component is what can cause the patient to experience a precipitated withdrawal.
A patient should stay on a maintenance dose of buprenorphine/naloxone (Suboxone®) for as long as it is helping. For many people that is years, not months.
Some patients do have a preference for the brand name. Most prescribers start generic and switch if the patient cannot tolerate it. It is hard to predict who will like/tolerate which version, especially since many patients are also having withdrawal symptoms, which can make it confusing as nothing tastes good when withdrawing from opioids.
Low-dose initiations (also referred to as micro induction) works well for any patient and is often the only option for those taking fentanyl.
No. While this was historically a requirement, evidence has since shown that buprenorphine treatment alone is effective at reducing morbidity and mortality. Do offer to connect patients to behavioral health treatment, but this should never be a barrier to a buprenorphine prescription.
Naltrexone and naloxone have the same mechanism of action but ONLY naltrexone is orally bioavailable. Naloxone is NOT.
Yes. Use caution with more advanced liver disease, but in most cases, naltrexone is safe. Have questions? Utilize OPEN’s consultation service and review these complex cases with our expert hepatologist!
Start buprenorphine/naloxone (Suboxone®), or methadone if working with an opioid treatment program (OTP).
Buprenorphine is compatible with breastfeeding. Naltrexone has not been studied well in pregnancy/breastfeeding so generally not recommended. There are a number of studies currently being done with the long-acting naltrexone in pregnancy.
Treating acute pain in someone who is taking long-acting naltrexone is very challenging. The patient will need more opioid medication to overcome the naltrexone blockage and full agonists are a better choice (hydromorphone usually). Encourage the patient to have a medical alert bracelet due to the risk of respiratory depression.
Yes, MOUD initiation can happen with a new patient on the first visit especially if a nurse or medical assistant can assist. The average visit is approximately 40 minutes, however there can be a wide range depending on office protocol.
No. There might be some requirements for telehealth-only, but those guidelines are still being finalized.
Yes, cravings are associated with return to use and sometimes, buprenorphine/naloxone (Suboxone®) is used in that situation. Recommendations would be to start at lower doses (for example 2-4mg total daily dose) because the patient doesn’t/won’t have the same level of opioid tolerance.
This Treatment Improvement Protocol (TIP) reviews the use of the three Food and Drug Administration (FDA)-approved medications used to treat OUD—methadone, naltrexone, and buprenorphine—and the other strategies and services needed to support recovery for people with OUD.
Collaborative care management of substance use disorders with emphasis on integration of low-barrier, evidence-based treatment utilizing medications for opioid use disorder. The focus of this most current guideline has expanded from Massachusetts and the Nurse, to a broader national audience of collaborative care teams including prescribers, recovery coaches, behavioral health team members, administration and support staff.
The primary care setting is a critical intervention point to increase diagnosis and treatment for patients with OUD. The American Academy of Family Physicians asserts that primary care providers’ delivery of patient-centered and compassionate care to diverse populations uniquely positions them to address the needs of patients with OUD. This resource document provides practical, evidence-based information for primary care providers and practices on prescribing buprenorphine to individuals in need of intervention. It discusses implementation considerations and strategies for primary care providers and primary care organizations to facilitate their understanding, planning activities, and implementation of buprenorphine prescribing.
Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment and an individual’s life experience.
A collection of clinical tools and form to use while working with patients with MOUD.
The purpose of these clinical guidelines is to provide detailed policies and protocols for the treatment of substance use disorder in pregnant and parenting patients utilizing buprenorphine and naltrexone formulations at Boston Medical Center.
The American Society of Addiction Medicine (ASAM) developed this National Practice Guideline for the Treatment of Opioid Use Disorder to provide information on evidence-based treatment of opioid use disorder.
The research on telehealth for mental health and other chronic conditions is extensive and has shown that overall, telehealth delivered care, including medication visits and psychotherapy, is no less effective than traditional in-person care in many situations.
The Disclosure of Substance Use Disorder Patient Records: How Do I Exchange Part 2 Data? fact sheet describes how 42 CFR Part 2 applies to the electronic exchange of healthcare records with a Part 2 Program.
On February 8, 2024, the U.S. Department of Health & Human Services (HHS) through the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Office for Civil Rights announced a final rule modifying the Confidentiality of Substance Use Disorder (SUD) Patient Records regulations at 42 CFR part 2 (“Part 2”). With this final rule, HHS is implementing the confidentiality provisions of section 3221 of the Coronavirus Aid, Relief, and Economic Security (CARES) Act – PDF (enacted March 27, 2020), which require the Department to align certain aspects of Part 2 with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Rules and the Health Information Technology for Economic and Clinical Health Act (HITECH).
This document is an educational document from the Substance Abuse and Mental Health Services Administration (SAMHSA) and the U.S. Department of Health and Human Services. It was prepared by SAMHSA staff, in collaboration with staff from the Office of the National Coordinator for Health Information Technology, and contractors and should not be considered legal advice.

Use this sample agreement as a starting point when prescribing buprenorphine.
This document offers a guideline to starting buprenorphine at a low dose.

This document is a guideline to starting buprenorphine at a standard dose.

Use this guide to help order urine testing and interpret the results.

This resource will help providers successfully provide withdrawal comfort and support.
The content on this page presented by the Overdose Prevention Engagement Network (OPEN) is intended solely to inform and educate healthcare professionals, and shall not be used for medical advice and is not a substitute for the advice or treatment of a qualified medical professional. For specific patient questions, submit a consultation request to OPEN.