Pediatrics Pain Management
Caregivers: Preparing for your child’s surgery can be overwhelming. To help you feel more confident, explore ways to manage their pain after surgery. On this page, see ideas on how to talk with your surgeon about what pain to expect. You can also find non-medication options to promote healing. Finally, learn how and when to use over-the-counter medications and opioids safely.
Providers: Support families with evidence-based guidelines for pediatric post-surgical pain management, including when to use opioids and alternatives. Use OPEN’s Pediatric Prescribing Recommendations, medication monitoring, and preoperative counseling to ensure every child’s recovery is safe, effective, and tailored to their needs.
This information is not meant to be applied in cases of chronic or long-term pain in children.
For Caregivers
Surgery can be stressful for both you and your child. This is natural and expected, and some of this comes from worry about the pain after surgery and how it can be managed. These tools will help you talk to your surgeon about pain before your child’s surgery and manage your child’s acute, or short-term pain following their operation.
Pain tells your child that their body is healing and that they might need to balance activity with rest. It is an uncomfortable but natural part of recovery. The amount of pain, how long it lasts, and when it peaks varies based on the procedure that the child has. Each child can have a different emotional response to pain as well, which changes their pain experience.
Preparing For Your Child's Surgery
Every child recovers from surgery in their own way, and kids who have the same procedure might have completely different experiences of pain. In most cases, the pain will not be long-lasting and will get better with time and healing. This is called acute pain. The goal with acute pain is to manage it in a safe way, so children can heal and recover well. This does not mean that your child will have no pain, but that your child’s pain should be tolerable. They should be able to drink, eat, and sleep as best as possible given their post-surgical condition. Pain can be managed using both medication and non-medication options as part of a larger pain management plan to be discussed with your surgeon.
Understand Expectations Around Pain After Surgery
Talk with the surgeon:
Getting answers to questions like these can help you navigate your child’s recovery with confidence. If your surgeon is using medical language that you don’t understand, ask them to rephrase it using common language.
- What level of pain is typical after this surgery?
- When should I expect the pain to improve?
- When should I be concerned if the pain doesn’t improve?
- What can I do to help the pain improve? Will over-the-counter medications such as Tylenol® (acetaminophen) and Motrin® or Advil® (ibuprofen) be recommended, and will you provide dosing instructions for them? Should I use them only if needed or on a schedule? Should I get them before surgery?
- Do you recommend prescription medication such as an opioid for my child? How much will you prescribe and at what dose? What are the risks of using an opioid?
- If I choose not to fill an opioid prescription for my child, will you honor that decision?
- If I don’t get an opioid prescription after surgery but then need it during recovery, how difficult is it to get later?
- Does the hospital have Child Life services who can offer preoperative experiences including tours and websites explaining the surgery process?
Be sure to mention:
- If your child has risk factors for opioid addiction, including depression, anxiety, current medication use, prior opioid misuse, or a family history of addiction
- If your child has increased anxiety about their surgery
- Any other concerns you may have about your child having surgery
Prepare With Your Child
Preparing for surgery together is important to help your child’s surgical experience and recovery go smoothly. Have age-appropriate conversations with your child about their planned surgery and what to expect. Consider your child’s anxiety level when talking to them about surgery.
- Let your child guide the conversation. Answer their questions as best as you can, using simple language they can understand.
- Choose the right time. If your child is anxious, it may be better to wait until a few days before surgery to discuss it with them, as their anxiety may grow as they wait. It is still very important to talk with them about surgery before the event, so they can be prepared.
- Check what resources your surgeon or hospital may have to help you prepare your child. Read stories of similar experiences – Thump! Ouch! is a book about a child who gets hurt and needs to go to the hospital. You can also watch videos as an example – Preparing for Surgery at Mott Children’s Hospital.
- Encourage feelings of security. Remind your child of the things that will stay the same despite the changes that happen with surgery and recovery. Some of these stable things include family, home, their room, pets, and their school. Help your child keep an attitude that is adaptive, flexible, and hopeful.
- Don’t be afraid to talk about pain. Help your child understand that you and the medical team will work to manage their pain as best and safely as possible. Be honest and positive. This will help your child have realistic expectations about their pain following surgery. Review the reasons for your child’s surgery, and remind them that the surgical pain will be temporary.
- After surgery, you might be invited to join your child in the recovery area. This will depend on your hospital’s policy. Know that some children are very upset when they first awaken. This can be a consequence of the anesthesia itself rather than pain. Your child’s recovery team is best equipped to manage this and can answer any questions you may have.
Create Comfort at Home
Your goal is to support your child and help them be as comfortable as possible. How will you know if your child is in pain? Ask them and watch them. You know your child best and can pick up on any signs that they’re in distress.
Pain might affect their sleep, appetite, and mood. They might wake up more often at night, not want to eat or drink, cling to you, or withdraw from you. For young children, it can be difficult to understand why they are having pain. Encourage and support them. Each child is unique, and their recovery may be different from another child’s. Use what you know about your child to help them recover.
Prepare Your Recovery Space
 Purchase the over-the-counter medications (Tylenol®, Motrin®, Advil®) that your care team has recommended to use at home.
Purchase the over-the-counter medications (Tylenol®, Motrin®, Advil®) that your care team has recommended to use at home.- Buy food and drinks that your care team recommends.
- Gather things such as toys, music, books, and technology to be used for distraction after surgery.
Prepare For Time Away From School
Your child may be at home and away from school or daycare for a period of time following surgery and may require your full-time care while they recover. If your child will miss school, communicate with their teacher before surgery to come up with a plan for their missed homework. If your child is anxious, this will also help reassure them that they won’t fall behind in their work.
Get Support Where You Can
Take good care of yourself, so that you are able to care for your child. Remember: pain is a typical response to surgery, and if your child has pain, this is the body’s natural way of recovering. If there are other members of your household who rely on you for care, try to create a plan that allows you time to focus on your child’s needs after surgery. Be sure to consider your own concerns about your child’s upcoming surgery and possible pain. Work to manage these, so you can be a calm, healing presence for your child.
Understand that if your child isn’t sleeping well, you probably will not be sleeping well either and may need support. Do not be afraid to ask for or accept help from others. Make a list of things that you could use help with, including:
- Groceries
- Pickups and care with other children
- Laundry
- Housecleaning
- Petcare
Non-Medication Pain Management
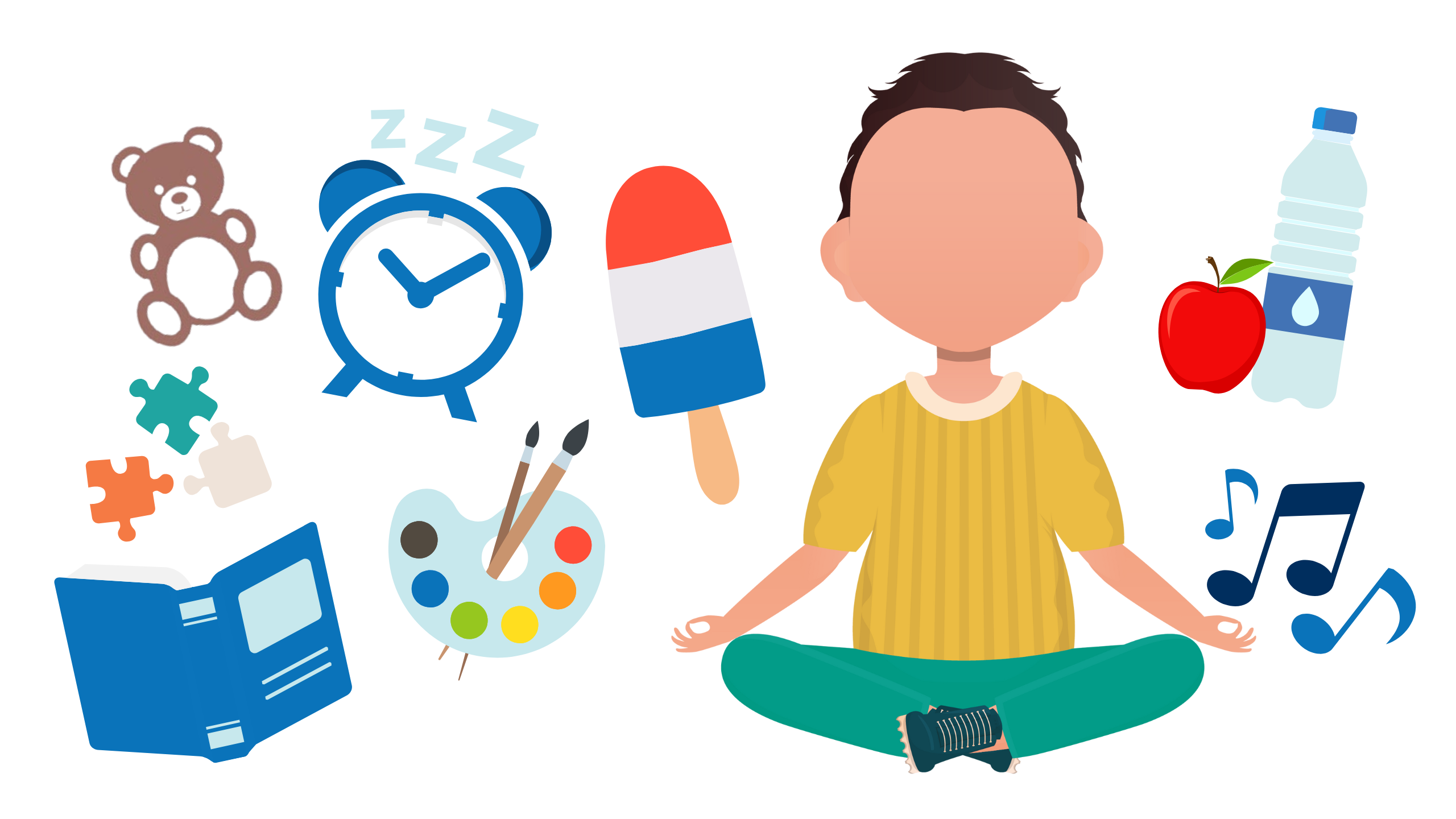
Helping children manage pain and discomfort involves more than just medicine. Non-medication strategies play an important role in supporting their physical and emotional well-being during recovery. Simple, comforting tools, like mindful breathing, music, special foods, or time with family, can help reduce anxiety, ease pain, and promote healing. These approaches can be used alongside the medications your surgeon has recommended and may even reduce the need for opioids and their potential side effects.
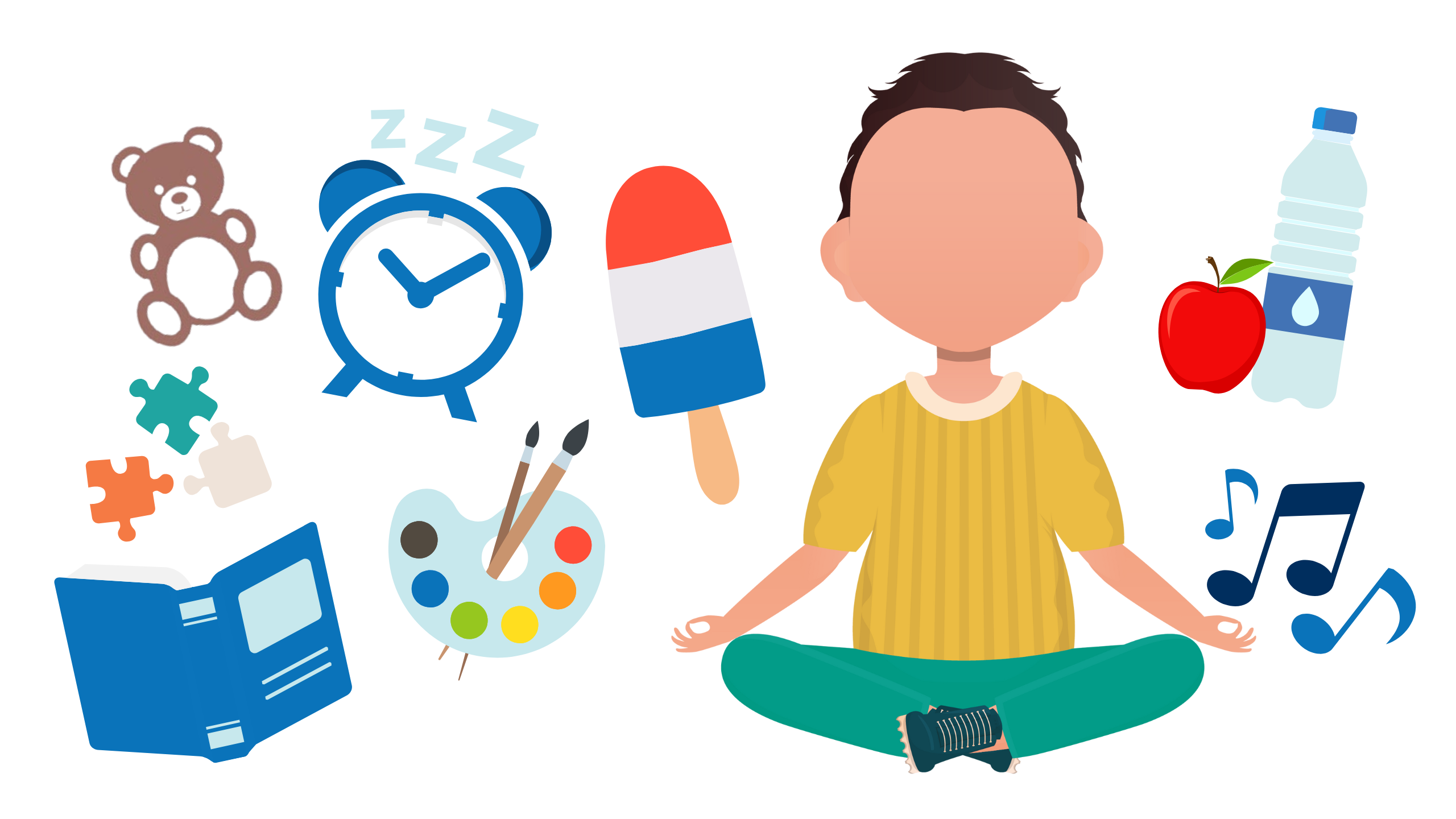
Pain Management Techniques
Give these a try to help manage pain after surgery.
- Mindfulness: Practicing calm breathing, like belly breathing or square breathing, can help to relax muscles that are tensed because of pain or anxiety. Your child can use their imagination to visualize a place that makes them feel calm, relaxed, and comfortable.
- Special Foods: Special foods, such as ice cream or popsicles, can distract your child from their pain by giving them something enjoyable to think about.
- Art: Art can be a tool for positive coping, a distraction from pain, and an outlet for your child or teen to communicate their feelings.
- Music: Music may be very comforting when your child is experiencing pain or discomfort. Listening to music, singing, or writing songs can help lessen pain and anxiety.
- Games & Play: Keeping your child’s mind focused on something else can help reduce their awareness of pain. Helpful distractions can include toys, board games, video games, or movies.
- Books: Reading children’s books about surgery and emotions can help your child understand their own pain and feelings better. This may give them a sense of control and decrease their anxiety. Reading your child’s favorite books and stories together can also comfort them.
- Family Time: Many children are reassured by the presence of their family. Spend time with your child and be a calming presence for them. Some children are relaxed by gentle touch and massage, which can help reduce pain.
- Sleep: Sleep helps the body heal. Allow your child to get the best night’s sleep possible by getting them to bed at their usual time and providing a relaxing and calm environment.
- Food & Hydration: Make sure your child is drinking enough fluids and eating as normally as possible while being mindful of any restrictions from your surgeon. Dehydration can worsen recovery and increase pain.
Non-Opioid Pain Medications
Your child’s surgeon may recommend using non-opioid medications such as Tylenol® (acetaminophen) and Motrin® or Advil® (ibuprofen). Tylenol® and Motrin® each work in different ways to manage pain. They can be given together.1
Give the dose your doctor recommends:
It is important to use the dose your surgeon recommends even if it is different from the dose listed on the medication bottle. The dose on the bottle is based on age, but dosing based on your child’s weight may manage pain better.
Your team may recommend using these medications on a regular basis (“around the clock”) to manage pain. This means giving your child the medications on a set schedule during the day and even at night. Ask your surgeon what dosing schedule to follow, as well as how to give the medications.
NOTE: Other medications may also contain acetaminophen. Check the labels on any medications you’re giving your child (such as a prescription opioid medication) to make sure they aren’t already receiving acetaminophen.
Let your care team guide you:
While these medications are usually alternated for management of fever, for pain they can be given together. If you give both Tylenol® and Motrin® together (at the same time), this decreases how often you need to give the medication and can be simpler. Follow the instructions your care team gives you in terms of how to use these medications and for how long. If taking the medications at the same time isn’t working well to control the pain near after 6 hours, consider alternating the medications.
Keep track of medications:
Keeping track of the medications taken is important. This will allow you to manage the pain safely without using more medication than is advised. As with any medications, there are possible serious side effects if used more frequently or at higher doses than prescribed.
You can keep track of medications by making notes on a medication log or on your phone. Write down the name of the medication, the time you gave it, the amount you gave, and when your child can have the next dose. Share this information with anyone else who is also caring for your child, so a dose isn’t accidentally given twice.
Tips for Giving Medication Safely
Try these methods when administering any type of pain medication to children.
Check
For liquid medications, check the concentration on the bottle to make sure you’re giving the correct milligram-based dose.
Comfort
Have a positive attitude. Be calm, honest, and empathetic but remain in charge. Explain why the medication is helpful.
Measure
Only use an oral syringe or medication cup to dose correctly. You can buy these at your pharmacy if they do not come with your medication.
Household spoons are not accurate to measure medications.
Praise
Give your child praise when they take the medication. Some children respond well to a small reward such as a sticker or a chart that leads to rewards.
Adapt
If your child resists taking the medication, use the syringe to squirt small amounts of medicine into the side of their cheek. This prevents gagging and your child is less likely to spit out the medication.
Be careful if you are mixing medication with a food your child enjoys in hopes of making it easier for them to take. If you do this, only mix the medication into a small spoonful of food. Otherwise, if they don’t finish it, you won’t know how much medication they took.
Consider
Ask your pharmacist if you can refrigerate the medication, as the cold temperature may make it easier for your child to take.
Sucking on ice chips or a popsicle first will also dull the taste of the medication. You can also follow the medication with a cold drink of something they enjoy.
Motrin® can cause stomach upset if taken without food. If possible, give with food or milk.
Opioid Medications
Opioids are strong prescription pain medications with the potential for serious side effects and complications. Common opioid names include oxycodone, hydrocodone, morphine, and codeine. Some opioids already contain acetaminophen. If this is the case, your child may be unable to take over-the-counter acetaminophen with the opioid. Check the label and discuss this with your pharmacist.
Use opioids for breakthrough pain:
To address acute pain, start by using non-medication strategies and non-opioid pain medications. Together, they are often enough to manage your child’s pain. In some cases, your child may have breakthrough pain, which is severe pain despite using non-medication strategies and non-opioid pain medications. Opioids can be used to manage breakthrough pain after surgery.
If your child receives a prescription for an opioid, it should usually only be used to manage their breakthrough pain. Know that even if you are using an opioid for breakthrough pain, you should still also use non-medication strategies and non-opioid pain medications. This will allow you to use as little of the opioid as possible.
Side Effects of Opioids
Anyone who uses an opioid is at risk for these potential side effects:
- Nausea and vomiting
- Constipation
- Itching
- Sleepiness
- Slowed breathing
- Impaired motor skills, thinking, or judgement
Children who are overweight or have obstructive sleep apnea or snoring have a higher risk of sleepiness or slowed breathing from an opioid. Do not use opioids to help your child sleep.
Constipation (difficulty having a bowel movement)
Impaired motor skills, thinking or judgment.
Opioids Have Real Risks
Anyone who uses an opioid, even for a short time, is at risk for dependence, tolerance, misuse, addiction, and overdose. Adolescents are especially at risk for opioid misuse and addiction because the parts of the brain that control impulsiveness and decision making are still developing.2 In addition, peer pressure can also affect their behavior. Other factors that increase the risk of opioid use disorder include personal history of depression and/or anxiety and family history of substance use disorder.
Tolerance
When an opioid no longer has the same effect on your child’s pain as it first did, which means they need a higher dose to control pain. For example, if your child is taking an opioid which first worked well for pain, and then later it doesn’t work as well, it does not always mean the pain is worse. Instead, your child may have become tolerant to the opioid.
Dependence
When your child’s body has started to rely on the opioid to function. This can happen even with using an opioid for a short time period, but the longer your child takes an opioid, the higher the risk. This is one reason why it is important to use an opioid for as short a time as possible. Suddenly stopping an opioid when a person is dependent causes symptoms of withdrawal, such as muscle aches, yawning, runny nose and tearing eyes, sweating, anxiety, difficulty sleeping, nausea/vomiting, and/or diarrhea.
Misuse
When your child takes the opioid they were prescribed at a higher dose, more often, or for reasons other than which it was prescribed.
Addiction
When your child develops a brain disease known as Opioid Use Disorder (OUD). People with this condition seek and use opioids even though they are causing them harm.
Overdose
When your child takes a dose of medication that is too high for them. This affects breathing and can cause your child to stop breathing.
Diversion
When anyone other than your child gets and uses the prescribed medication. This can happen when you do not safely dispose of an opioid or leave it unattended. Diversion is dangerous because it can lead to misuse, overdose and/or opioid use disorder in others. Sharing or selling an opioid is a felony in the state of Michigan.
Reduce Opioid Risks
Use these strategies to reduce risks associated with opioids:
- Tell your doctor about any other medications your child is taking and if your child has a history of opioid misuse or addiction, depression or anxiety, or a family history of addiction.
- Do not use opioids along with antihistamines such as Benadryl or sleep medications.
- Only use the opioid for the reason, dose, and frequency that it was prescribed, and use it for the shortest possible time period. If your child doesn’t need it, don’t use it and dispose of it properly.
- Write down what medications you’re giving your child and when. This will help you be sure you’re using the medication only as prescribed.
- Double-check dosing to make sure you’re giving only the amount prescribed.
- Watch your child for signs of side effects or complications, and if you notice them, contact your provider.
- Lock the opioid medication in a safe place. If you cannot lock it up, keep it out of common areas of the house.
- Do not share your child’s opioid with anyone else. It is a prescription only for your child.
- Dispose of any remaining medication in a safe way when your child has recovered. Keeping an opioid prescription in your home is risky. Children may accidentally take it and overdose, and others may find it and misuse it. Ask your pharmacy if they have home drug deactivation/disposal kits to give you so you can safely dispose of your medication.
Healthcare Providers
When preparing to perform any kind of surgery on a pediatric or adolescent patient, providers must be prepared to help the patient and their families understand all of the options when it comes to postoperative pain management. With OPEN’s resources on hand, providers will be able to understand when to prescribe opioids or non-opioid medications, be able to inform other Primary Care Providers (PCPs) about the patient’s surgery and pain management plan, and most importantly, educate the family on all available options.
Perioperative Best Practices
A multidisciplinary working group at Michigan Medicine with representatives from Surgery, Anesthesiology, Nursing, Pharmacy, Child Life, and Psychology, who provide care for patients and families after surgery developed these best practices.

Throughout the Perioperative Pathway
Provide a consistent message about pain management and medication use, risks, storage, and disposal. Make sure that verbal and written instructions from all providers are consistent, from preoperative evaluation to postoperative follow-up. Coordinate transitions between all clinicians to establish shared expectations for postoperative recovery and pain management needs.
Preoperative Counseling
As early as possible before surgery, discuss expectations regarding the experience of pain, length of recovery, and functional pain management goals with the patient and family in an age-appropriate manner. Do not routinely provide opioid prescriptions intended for postoperative use prior to surgery.
Intraoperative Considerations
Discuss with the anesthesia team how to best manage the patient’s pain in the operating room so postoperative pain is minimized. Think about using a nerve block, local anesthetic catheter, or epidural when appropriate. Administer intravenous non-opioid medications (e.g., ketorolac, acetaminophen) for management of pain before arrival in the postanesthetic care unit unless contraindicated.
Immediate Postoperative Considerations
In the recovery area, use nonpharmacologic techniques such as distraction, Child Life services, and parental presence to address pain and anxiety as soon as it is safe to do so. When appropriate, give enteral non-opioid medications if not already administered pre- or intraoperatively. If opioids are used in the recovery area, oral administration is preferred over IV administration. Consider obtaining a consult from the Pain Service if the patient’s pain is poorly relieved despite standard therapy or from the Pediatric Psychiatry Service if a new history of substance use disorder is identified in a patient.
Postoperative Discharge Considerations
Use non-opioid therapies as a primary method for pain management and include dosing of over-the-counter (OTC) medications and instructions for their use. Discuss and encourage non-pharmacologic therapies, including distraction, heat or ice, and physical therapy.
Primary Pain Medications
Acetaminophen (Tylenol®) and ibuprofen (Motrin®, Advil) can provide similar pain management to opioids. Specifically, a randomized study on pediatric patients undergoing tonsillectomy and adenoidectomy, a procedure associated with significant postoperative pain, showed that ibuprofen and acetaminophen in combination provided similar analgesia to morphine without risk of respiratory depression.3
Patient-reported outcome data collection by OPEN also show that for procedures such as circumcision, herniorrhaphy, appendectomy and adenoidectomy, patients have adequate pain management with acetaminophen and ibuprofen alone.4 Even if opioids are prescribed, using medications such as acetaminophen and ibuprofen can decrease opioid use.
Prescribe Acetaminophen and Ibuprofen
Since acetaminophen and ibuprofen are available over the counter and don’t require a prescription for patients to use, patients and caregivers often do not receive instructions on how to use them after surgery. The packaging instructions for acetaminophen and ibuprofen provide dosing for an age and weight range and recommend as-needed use. If families follow these instructions, they may be under-dosing their children and inadequately addressing their pain. And if they were prescribed an opioid, they may think this is the first medication they should use for their child’s pain, not understanding that acetaminophen and ibuprofen often provide adequate pain relief when dosed and administered correctly and that an opioid may not be needed.
At Michigan Medicine, acetaminophen and ibuprofen are sent electronically as prescriptions to a patient’s pharmacy. When acetaminophen and ibuprofen are written as prescriptions and instructions on how to use them are provided, families then have clear information regarding dosing and understand these are the first-line medications for pain management. Some insurance companies may also cover the cost of these medications when they are written as a prescription.
How To Dose Acetaminophen and Ibuprofen
- For mild pain, these are used either individually or together on an as-needed basis.
- For moderate pain, they are given on a schedule together every 6 hours during the day, and at night as needed (if the patient wakes) for 1-2 days after surgery, and then as needed.
- For severe pain, they are given on a schedule together around the clock for 2 days after surgery and then as needed.
ACETAMINOPHEN
- 15 mg/kg every 6 hours
- Maximum dose of 1000 mg per dose
- Also called Tylenol
IBUPROFEN
- 10 mg/kg every 6 hours
- Maximum dose of 800 mg per dose
- Also called Motrin
Give Acetaminophen and Ibuprofen Together
Many families are familiar with using acetaminophen and ibuprofen on an alternating basis as needed for fever and assume they should use them for pain control in the same way. However, from a pain management standpoint, the half-life of both of these medications is long enough that they can be given together.
Giving these two different medications at the same time has benefits:
- Much simpler for families
- Decreases the likelihood of missing or duplicating a dose
- Less disruptive to both sleep and daytime schedules
Simultaneous administration may also allow for longer-lasting pain management. Provide caregivers with information about how to administer these two medications.
NOTE:
- Avoid ibuprofen and other non-steroidal anti-inflammatory drugs (NSAIDs) in patients with bleeding disorders, renal disease, peptic ulcer disease, and for specific operations at surgeon discretion.
- Do not use ibuprofen in children under 6 months of age.
- Use only one NSAID at a time (do not combine NSAIDs).
- Use caution when prescribing acetaminophen in patients with hepatic impairment or active liver
Streamline Prescribing and Education by Using Order Sets
When patients are discharged after surgery, providers can benefit from premade discharge order set that contains instructions on postoperative care. Standard orders for acetaminophen and ibuprofen and instructions on their use can be added to the postoperative order sets. This simplifies the process of prescribing for providers and removes the barrier of additional work.
It also allows for standard weight-based dosing and instructions and offers the opportunity for families to receive the medication at a pharmacy (where it may be covered by insurance). Providing the medications as a prescription validates these over-the-counter medications as the first-line choice for pain management and ensures patients receive the appropriate dose for their size.
Sample Order Set: Patient Education
If medication is needed to manage your child’s pain after surgery, the best medications to begin with are over-the-counter pain medicines. These are acetaminophen (example: Tylenol®) and ibuprofen (example: Motrin® or Advil®).
- Do NOT give ibuprofen to children under 6 months of age or if your child’s doctor has told you not to use it.
- Do NOT give any medications in higher amounts or more often than instructed.
If your child is prescribed both Tylenol and Motrin, the best way to control their pain is to give the medications TOGETHER every 6 hours.
- Start with a dose of Motrin® and Tylenol® together
- 6 hours later give another dose of Motrin® and Tylenol® together
Tips for giving medication safely:
- For liquid medications, check the concentration on the bottle to make sure you’re giving the correct milligram-based dose.
- Only use an oral syringe or medication cup to dose correctly. If a dosing tool does not come with the medication, ask the pharmacy for one.
- Household spoons are not accurate to measure medications.
- If your child resists taking the medication, use the syringe to squirt small amounts of medicine into the side of their cheek. This prevents gagging and your child is less likely to spit out the medication.
- If your child is resistant to taking pain medication, you may try mixing it with a food or syrup your child enjoys. Some mixes that have worked for other children include mixing medicine with a popsicle to make a slushy or adding chocolate syrup or applesauce.
- Be careful if you are mixing medication with a food your child enjoys in hopes of making it easier for them to take. If you do this, only mix the medication into a small spoonful of food. Otherwise, if they don’t finish it, you won’t know how much medication they took.
- You can also use other non-medication approaches to manage your child’s pain. These include spending time with them, playing or doing special projects, eating special foods, watching their favorite shows or movies, and using a cold or warm pack.
Patient-Specific Opioid Prescribing
In cases that call for an opioid prescription, employ strategies to ensure that patients and caregivers are well-informed about the appropriate usage and risks. Tailoring prescribing to help reduce your patient’s risk of developing persistent opioid use, as well as connecting patients to resources, can help ensure safer opioid use during their post-surgical acute pain management.
The following best practices were adapted from the Prescription Drug and Opioid Abuse Commission (PDOAC) prescribing recommendations, which were created in partnership with OPEN and the University of Michigan Injury Prevention Center.5 These strategies have been implemented at Michigan Medicine since 2019.
Screen for the patient’s opioid-related risk by looking for the following factors:
- Increased risk of respiratory depression: Concurrent medication use (e.g., prior opioid prescriptions, sleep aids, benzodiazepines), obstructive sleep apnea, obesity, neurological disorder, oxygen desaturation prior to discharge.
- Increased risk of opioid misuse: Concurrent medication use (e.g., prior opioid prescriptions, sleep aids, benzodiazepines), depression, anxiety, chronic pain, past prescription misuse, substance use, or substance use disorder.
Educate patients and families about:
- Use of prescription opioids ONLY to manage severe breakthrough pain that is not relieved by acetaminophen and ibuprofen
- How to taper opioid use as pain improves
- The side effects of opioid medications (sedation, respiratory depression, dependence, withdrawal)
- The risks of opioid medications, which include addiction, overdose, and diversion (use by anyone other than to whom it was prescribed)
- How to safely store and dispose of opioids
- Appropriate use of naloxone, if prescribed
Coordinate postoperative care transitions with primary care providers for patients with elevated risk.
- Refer patients to a specialist for management of substance use disorder or chronic pain, if appropriate.
- Use language that respects individuals with substance use disorder to mitigate stigma.
- If a patient screens positive for increased risk, provide the patient and family education regarding possible adverse outcomes and establish a follow-up plan. The prescription drug monitoring program (PDMP) must be accessed prior to prescribing controlled substances in schedules 2-5 when exceeding a 3-day supply, in compliance with Michigan law.
NOTE:
- Do NOT prescribe codeine or tramadol. Due to pharmacogenetic differences, codeine and tramadol are poor choices for pain management and should not be prescribed.
- Do NOT prescribe fentanyl or long-acting opioids (e.g. methadone, OxyContin®).
- AVOID prescribing opioids that contain acetaminophen (e.g. Norco®, Vicodin®, Percocet®) to minimize risk of acetaminophen overdose.
- AVOID prescribing opioids with other sedative medications (e.g., benzodiazepines, skeletal muscle relaxants).
- If concurrent prescribing is necessary (e.g., to manage postoperative muscle spasms), educate the patient and family about the increased risks of sedation and respiratory depression and consider co-prescribing naloxone.
Opioid Prescribing Recommendations
OPEN conducted a survey of caregivers for pediatric (under 18) postoperative patients at Michigan Medicine from 2020 through 2022. Over 1,000 surveys have been completed for pediatric patients undergoing a variety of surgical procedures through spring 2022. Procedures were selected based on the frequency with which they occurred and/or associated opioid prescriptions.
Eligible patients and their caregivers were called to ask about the quantity and duration of opioid use, use of over-the-counter pain medications, pain score, and overall satisfaction with post-surgical pain management. Patient demographic information, procedure type, and opioid prescription data were gathered from electronic health records and matched with survey information to analyze prescribing patterns, compare pain management, and assess for evidence of overprescribing.
OPEN has published fourteen evidence-based pediatric prescribing recommendations across 5 surgical specialties, including dental, general, otolaryngology, plastics, and urology surgery. These recommendations serve as a starting point for discussions with the patient and their caregivers around pain management using opioids. For more information on using these recommendations in your practice, visit OPEN’s Opioid Prescribing Recommendations page.
Learn How to Use Our Prescribing Recommendations
Case Study: Circumcision
Patient Cohort
- 114 pediatric patients
- Pain addressed with acetaminophen and ibuprofen
- 1 patient prescribed an opioid
- 65% survey response rate
Lessons Learned:
Nearly Zero Opioids Prescribed: For the 114 patients undergoing circumcision during the quality improvement period, only one patient was prescribed an opioid for pain management.
Pain and Pain Expectations Were Managed: Parents reported that pain after surgery was mostly mild to moderate. On the scale of 1 to 5, 1 being no pain and 5 being worst possible pain, the median pain reported was 2.5. Notably, even parents of children experiencing pain did not report dissatisfaction with pain management. Nearly all parents reported their child’s pain being about what they expected or better than they expected.
Parents Satisfied with Pain Management: Nearly all parents of children undergoing circumcision in the project period reported satisfaction with their child’s pain management.
Preoperative Medication Counseling
As prescribers write for fewer opioids, there may be concern about possible increase in phone calls for refills or inadequate pain management. In fact, single institution studies found that with appropriate patient education, not only did patients consume less medication, but requests for refills did not increase.6 To ensure appropriate pain management, all patients and families should receive preoperative counseling about postoperative pain and how to manage it.
Set Clear Expectations
Talk about the experience of pain and usual length of recovery with the patient and family in a manner that is age appropriate.
“Some pain is normal. Your child should be able to walk and do light activity but may be sore for a few days. This will gradually get better with time.”
“Half of all patients who have this procedure take less than five doses of an opioid medication.”
Discuss Effective Alternatives
Discuss use of over-the-counter medications.
“Tylenol® and Motrin® are the first medications we use to manage your child’s pain after surgery. By themselves, they are often enough to manage your child’s pain.”
Explain Safe Use
Explain when opioids should be used.
“These pills are only for management of severe pain from your child’s surgery and should not be used to manage pain from other conditions.”
Talk About Risks
Talk about the possible risks associated with opioids.
“We are careful about opioids because they have been shown to be addictive, cause harm, and even cause overdose if used incorrectly or abused.”
Advocate for Disposal
Let patients know that they should dispose of their medications after acute post-surgical pain has resolved, and how they should do this.
“Disposing of the opioid prevents accidental overdose or misuse. You can use a drug disposal bag, take pills to an approved collector (including police stations), or mix the medication with kitty litter in a bag and throw it in the trash.”
Weight-Based Dosing

In children, opioids are prescribed based on weight (mg/kg) up to a maximum weight of 50 kg. However, most oral opioids have a small volume of distribution and are not well absorbed by fat. If obese children are dosed based on their actual weight, they are at greater risk for complications or side effects compared to children in a lower weight category. In addition, a number of overweight and obese children have comorbid sleep-disordered breathing and are already at higher risk for respiratory complications related to opioid use.
How should opioids be prescribed for overweight and obese children to ensure they do not receive higher doses than are safe?
Optimally, body mass index (BMI) would be considered when dosing opioids. If BMI falls outside of the healthy weight range, providers should not follow strict weight-based dosing and instead consider using ideal body weight, lean body mass or lower dose per kg reference. A recent review performed at Michigan Medicine shows that children with BMI in the overweight and obese categories are receiving more morphine milligram equivalents compared to their peers who fall into a healthy weight category.7 Further research is necessary to determine how to best calculate opioid dosing in overweight and obese children.
Check Prescription Monitoring Programs

Prescription drug monitoring programs (PDMPs) are state-level electronic databases that track prescriptions for controlled substances such as opioids.8 All 50 states and the District of Columbia have implemented PDMPs in an effort to improve risky opioid prescribing practice and keep patients safe and informed.9
In Michigan, the PDMP is the Michigan Automated Prescription System (MAPS). Michigan law requires that a query of MAPS be performed when an opioid supply of three days or more is prescribed for a patient. It is good practice to check MAPS prior to prescribing any opioid or controlled substance, regardless of duration.
Once every quarter, the Michigan Department of Regulation and Licensing sends providers a report of the controlled substances they have prescribed for patients. To assess for ongoing use in patients who have received new opioid prescriptions, consider checking another MAPS report on the patients on your report.
Connect with Primary Care
While a prescription from a surgeon may be the initial point of opioid exposure for a patient, the relationship a surgeon has with a patient is often episodic. As a result, signs of ongoing use or misuse may not be identified. A primary care provider has a longitudinal relationship with the patient and can be better equipped to identify persistent use, misuse, or onset of substance use disorder. However, primary care providers are often unaware that their patients have received an initial opioid prescription from their surgeon. Providing a primary care provider with information about their patient’s operative procedure and the plan for management of acute postoperative pain (especially if that plan includes an opioid prescription) allows for better communication, consistent messaging, and improved patient monitoring after surgery.
The goal of this communication is to let the primary care provider know:
- That their patient had surgery,
- When the surgery occurred,
- The plan for pain management,
- If an opioid was prescribed and, if so, how much was dispensed, and
- The expectations in terms of pain duration and plan for refills (if any).
Ideas in terms of sharing this information include using the capability of the electronic medical record to auto-populate a letter or communication to the primary care provider containing this information. If an after-visit summary is created by your electronic medical record, you might forward a copy of this automatically to the primary care provider. Providers could also add standard language to their operative notes containing this information and forward the operating report to the primary care provider.
Featured Resources
Resources
Programs
References
- Daniel R. Jensen, Pharmacologic management of post-tonsillectomy pain in children, World Journal of Otorhinolaryngology – Head and Neck Surgery, Volume 7, Issue 3, 2021, Pages 186-193, ISSN 2095-8811, https://doi.org/10.1016/j.wjorl.2021.03.004.
- National Institute on Drug Abuse. (2022, March 4). NIDA for Teens. National Institute on Drug Abuse (NIDA). Retrieved March 18, 2022, from https://teens.drugabuse.gov/
- Lauren E. Kelly, Doron D. Sommer, Jayant Ramakrishna, Stephanie Hoffbauer, Sadaf Arbab-tafti, Diane Reid, Jonathan Maclean, Gideon Koren; Morphine or Ibuprofen for Post-Tonsillectomy Analgesia: A Randomized Trial. Pediatrics February 2015; 135 (2): 307–313. https://doi.org/10.1542/peds.2014-1906
- Harbaugh CM, Vargas G, Streur CS, et al. Eliminating Unnecessary Opioid Exposure After Common Children’s Surgeries. JAMA Surg. 2019;154(12):1154–1155. doi:10.1001/jamasurg.2019.2529
- Opioid Commission releases acute pain prescribing recommendations for Health Professionals. OPEN. (n.d.). Retrieved March 18, 2022, from https://michigan-open.org/opioid-commission-releases-acute-pain-prescribing-recommendations-forhealthprofessionals/
- Patient counseling. OPEN. (n.d.). Retrieved March 18, 2022, from https://michiganopen.org/patient-counseling/
- Unpublished institutional data. Publication will be provided.
- Substance Abuse and Mental Health Services Administration. (2017). Prescription Drug Monitoring Programs: A Guide for Healthcare Providers. In Brief, 10(1). https://store. samhsa.gov/sites/default/files/d7/priv/sma16-4997.pdf
- Issues at a Glance: Prescription Drug Monitoring Programs (PDMP). American Association of Nurse Practitioners. Accessed June 27, 2024. https://www.aanp.org/advocacy/advocacyresource/policy-briefs/issues-at-a-glance-prescription-drug-monitoring-programs-pdmp
Disclaimer: This information is not meant to be applied in cases of chronic or long-term pain in children.