OPEN Teen was developed with a group of young people dedicated to helping peers understand and navigate opioids and pain management effectively. Our goal is to create a supportive community where we can openly discuss the challenges and solutions surrounding opioid use. On this site, you’ll find answers to essential questions like what an opioid is and in-depth information is about what the opioid crisis is.
Ever wondered where opioids are found or how you could potentially recognize if someone you know is dealing with opioid use? Our resources will guide you on how you can help suspected opioid use and provide crucial steps on what to do if someone is experiencing an overdose. Talking about opioids can be tough, but it doesn’t have to be. We offer practical advice on how to talk about opioids easier so you can approach these conversations with confidence and care. Together, we can make a difference by staying informed and supporting each other through this important issue.

Opioids are a type of drug with powerful pain-relieving properties. Opioids can include medications prescribed by a doctor or illicit (illegal) drugs.
Opioids reduce feelings of pain and can cause feelings of intense happiness.
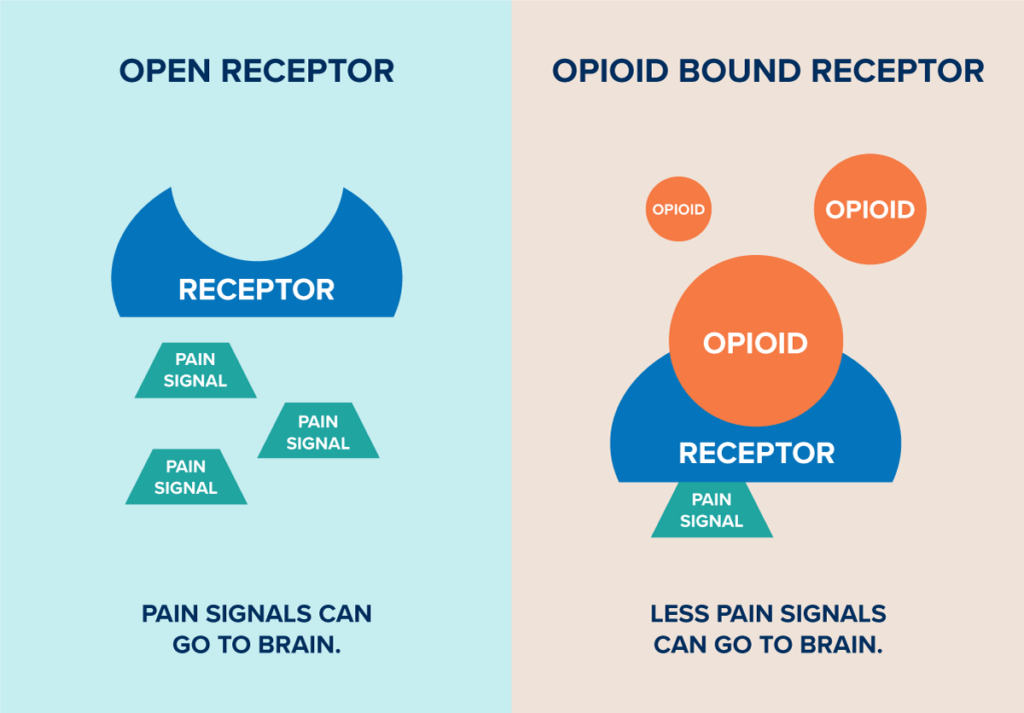
When opioids are put into the body, they move around in the bloodstream. When they find specific opioid receptors, they bind to them. This attachment blocks the receptor from sending pain signals from the body to the brain. This is why opioids can be very effective in managing pain after surgeries or injuries, or for people suffering from chronic pain.
Opioids also affect the part of the brain involved in reward. When someone takes opioids, they can experience a sense of euphoria or intense joy. The brain may start to rely on opioids to feel pleasure, creating a strong desire to keep using them despite harmful consequences. This is how addiction can start. Over time, larger and larger amounts of opioids are needed to get the same level of pleasure, which increases the risk of overdose.
Three kinds of opioids exist. Each type of opioid has the potential to be used medically for pain relief, but they all also carry significant risks of overdose and addiction.
Other medications such as acetaminophen (Tylenol®) or ibuprofen (Advil® or Motrin®) can help manage pain by blocking pain signals. While acetaminophen and ibuprofen can have risks if they are taken inappropriately, they are generally viewed as being safe when used at the correct dose, and do not have addictive properties. This is different from opioids that function through specific receptors and can become desensitized when too much opioid is present. There are also ways to manage pain without medication, such as using distraction techniques.

Natural Opioids
These are derived directly from the opium poppy plant and include morphine and codeine. They are the least processed of the opioid types.
Semi-Synthetic Opioids
These are created in scientific labs from natural opioids and are modified versions of the natural compounds found in opium.
Synthetic Opioids
These are completely made in a laboratory. Synthetic opioids are often stronger than other opioids because they are chemically engineered to more effectively bind to receptors in the brain and nervous system.
Here is a comprehensive table listing various opioids, including their commercial or prescription names, alternate names, common forms, and typical methods of administration. This table is designed to help you quickly identify different opioids and understand how they are commonly prescribed and used.
| Commercial/Prescription Name | Alternate Name1 | Common Forms2 | Common Ways Taken2 |
|---|---|---|---|
| Oxycodone, OxyContin®, Percodan®, Percocet® | O.C., Oxycet, Oxycotton, Oxy, Hillbilly Heroin, Percs | Capsule, liquid, tablet | Swallowed, snorted, injected |
| None. More information: NIDA | Heroin Brown sugar, China White, Dope, H, Horse, Junk, Skag, Skunk, Smack, White Horse, With OTC cold medicine and antihistamine: Cheese | White or brownish powder, or black sticky substance known as “black tar heroin” | Injected, smoked, snorted |
| Fentanyl, Actiq, Duragesic, Sublimaze | Apache, China Girl, China White, Dance Fever, Friend, Goodfella, Jackpot, Murder 8, Tango and Cash, TNT | Lozenge, sublingual tablet, film, buccal tablet | Injected, smoked, snorted |
| Codeine | Captain Cody, Cody, Lean, Schoolboy, Sizzurp, Purple Drank With gluteth- imide: Doors & Fours, Loads, Pancakes and Syrup | Tablet, capsule, liquid | Injected, swallowed (often mixed with soda and flavorings) |
| Hydrocodone, Vicodin®, Lortab®, Lorcet® | Vike, Watson-387 | Capsule, liquid, tablet | Swallowed, snorted, injected |
| Hydromorphone, Dilaudid® | D, Dillies, Footballs, Juice, Smack | Liquid, suppository | Injected, rectal |
| Meperidine, Demerol® | Demmies, Pain Killer | Tablet, liquid | Swallowed, snorted, injected |
| Methadone, Dolophine®, Methadose® | Amidone, Fizzies With MDMA: Chocolate Chip Cookies | Tablet, dispersible tablet, liquid | Swallowed, injected |
| Morphine, Duramorph®, Roxanol® | M, Miss Emma, Monkey, White Stuff | Tablet, liquid, capsule, suppository | Injected, swallowed, smoked |
| Oxymorphone, Opana® | Biscuits, Blue Heaven, Blues, Mrs. O, O Bomb, Octagons, Stop Signs | Tablet | Swallowed, snorted, injected |
Yes. The strength of an opioid is determined by how attracted it is to receptors in your body and how it affects them. Fentanyl is a common synthetic opioid, which is up to 50 times more potent than heroin or up to 100 times stronger than morphine.3 Strong drugs like fentanyl require much smaller doses to have an effect compared to natural opioids. This means that the lethal dose is much smaller, which increases the risk of overdose. Strong opioids can also have a higher risk of developing tolerance and dependence, as the body may adapt more quickly to the powerful effects of these drugs, which can lead the user to take higher and more frequent doses to achieve the same effect, further escalating the risk of addiction and overdose.
While opioid medications can be effective for pain management when used as directed by a healthcare provider, they can be harmful and dangerous – especially when misused. Opioid misuse could look like using more than the amount prescribed, using more frequently than prescribed, or using opioids that were not prescribed to you.
Most people who take prescription opioids do not become addicted or experience an overdose. The risks of opioid use in young people are particularly concerning due to their developing brain and the potential for long-term consequences. Here are some specific risks associated with opioid use in teenagers:
Using opioids carries a risk of addiction, but not everyone who uses them will become addicted. Chances of addiction are influenced by how long the opioids are used, how much is used, as well as individual biology, genetics, and environmental factors. To minimize the risk of addiction, it is crucial to use opioids only as directed by your healthcare professional. It is important to have a conversation with your healthcare provider about the risks and benefits of an opioid prescription.

Learn how to help manage or reduce your pain and anxiety through various techniques.
Over time, regular use of opioids can lead to tolerance, where higher doses are needed to achieve the same effect, which can subsequently increase the risk of addiction and overdose.
Adolescents have a risk of developing addiction more quickly than adults because their brains are more susceptible to the rewarding effects of drugs. Teenagers who misuse prescription opioids are also at a greater risk of transitioning to more risky drug use in the future.
The teenage brain is still developing. During adolescence, the brain goes through a healthy “pruning” process where unused connections between brain cells are removed to make way for more complex decision making in adulthood.4 Opioid use can disrupt the normal maturation process, leading to potential cognitive and emotional dysfunction.
Teenagers may not be aware of the potency of opioids or the risks of combining them with other substances. Overdose risk can be higher due to inexperience, potential for misuse, and the possibility of encountering illicit opioids that are stronger than anticipated. Overdose can be non-fatal, with many possible side effects, or fatal, which results in death.
Physical dependence can develop with chronic use of opioids, leading to withdrawal symptoms upon abrupt discontinuation or reduction of the drug. These symptoms can include severe flu-like symptoms, agitation, anxiety, and cravings.
Combining opioids with other substances, especially central nervous system depressants like alcohol, benzodiazepines, or other medications that cause drowsiness, can increase the risk of life-threatening respiratory depression, or slowed breathing.
Opioid misuse among teenagers is associated with mental health issues, including increased levels of depression, anxiety, and suicidal ideation. Long-term opioid use can also result in a variety of physical health issues such as hormonal dysregulation, immune system suppression, constipation, and nausea.
Teenagers using opioids may engage in riskier behaviors, such as unprotected sex or driving under the influence. Significant consequences include sexually transmitted infections (STIs), unplanned pregnancies, and car accidents.
If taken while pregnant, opioids can cause neonatal abstinence syndrome (NAS), a condition where a baby is born with opioid dependence and has withdrawal symptoms after birth.
Misuse of opioids can lead to significant social consequences, including job loss, legal issues, strained relationships, and social isolation.
Opioid misuse can interfere with normal social interactions and educational progress. It can lead to decreased academic performance, missing school, a higher dropout rate from school, and difficulty building healthy relationships.
Being caught with opioids without a prescription can lead to legal issues, which can alter a teen’s life course significantly. Early encounters with the criminal justice system can have lasting impacts on education, employment, and long-term life opportunities.
Preventing opioid misuse includes education about the risks, proper medication management, and increased awareness. If you are prescribed opioids for a medical reason, they should be closely monitored, and their use should be limited to the shortest amount of time possible. Pain management strategies without using medications and over the counter pain medications should be used to lower the risks associated with opioid use in this vulnerable population.


The opioid crisis is a complex public health issue that was declared an emergency by the US Government in October 2017. 5 Opioid misuse and overdose are happening across the entire population, including in teens, adolescents, and young adults.6 Doctors prescribing excess opioids, not teaching people early enough about the risks of opioids, and illegal drugs like fentanyl being more available are some major reasons why the opioid epidemic exists. It can also be hard to find care and expensive to access treatment when someone has concerns about their substance use and expensive to access treatment.
Beginning in the late 1990s, there was a large increase in prescribing opioid medications. Pharmaceutical companies reassured the medical community that patients would not become addicted to opioid pain relievers, which led to in excess and unnecessary opioid prescribing.7
Initially, there was insufficient education for both healthcare providers and patients about the risks associated with opioid use, including the potential for addiction and overdose. Without adequate education and intervention strategies, the risk of people transitioning from prescription opioid misuse to opioid use disorder (OUD) was underappreciated.
The rise of illegal opioid manufacturing and distribution, such as fentanyl, has greatly worsened the crisis. Fentanyl is much more potent than heroin or morphine and can be mixed with other drugs without users’ knowledge, leading to a significant increase in overdose deaths.
Overdose rates can also be influenced by other factors such as changes in the drug market and availability of stronger substances, the impact of the COVID-19 pandemic on mental health and substance use, and the availability of treatment and harm reduction services.
Just as there are many different causes of the opioid epidemic, tackling the crisis requires addressing the issue at all the different levels. This includes primary prevention, harm reduction, access to treatment, and supporting recovery.
Yes. The opioid epidemic in Michigan mirrors the trend across the United States, with a sharp increase in opioid-related overdoses and deaths in recent years. In Michigan, opioid deaths have increased by ten times the amount since 2000, fueled by rises in prescription opioid misuse, increases in heroin use in 2010, and the emergence of fentanyl in 2013.

Many adolescents and young adults encounter opioids for the first time when they are prescribed by their doctor. You may get a prescription to help manage your pain after a major surgery or dental procedure, such as getting your wisdom teeth removed.8 Examples of opioids you may get prescribed include Oxycodone, Percocet, Hydrocodone, or Codeine (see What Is an Opioid above for more information).
Addiction isn’t limited to the people using illegal opioids, such as heroin. Regular use of opioids, even as prescribed by a doctor or medical professional, can lead to dependence. Misuse includes people with a prescription not taking it as prescribed–taking too many pills at once, for example–or people without a prescription taking pills they get from a family medicine cabinet, friends, random strangers at a party or drug dealers selling pills illegally.9
There are many reasons one may take a prescription opioid. One of the most important things to remember is to have a conversation with your provider about safe use practices, non-opioid options and non-medication pain management strategies.
Talking to Your Doctor About an Opioid Prescription
It is important to have a conversation with your doctor if you think the pain medicine, they are prescribing is an opioid. You should discuss the benefits and risks of taking an opioid with your doctor and make a plan for disposing of any leftover opioids you may have once your short-term (acute) pain is gone. You can also ask for alternative treatment for pain or ask for a limited prescription so you don’t have pills that you will need to dispose of later.
Examples of questions you can ask your doctor:10

If you are having a surgical procedure, you can also use a Pain Plan Tool to help you identify the different pain management options you have and what other issues you should consider before the surgery takes place.
Illegal drugs such as heroin or illicit fentanyl are other sources of opioids.
Illegal drugs can have added risks because there is no official oversight or quality control, which means you may have no way of knowing what else has been added to a pill, or whether it contains a lethal dose of fentanyl.
It is important to remember that fentanyl can’t be seen, tasted, or smelled, so it’s almost impossible to tell if the drugs have been contaminated unless they are tested with fentanyl test strips. Fentanyl test strips are small strips of paper that can detect fentanyl in all different kinds of drugs (cocaine, methamphetamine, heroin, etc.) and drug forms (pills, powder, and injectables). The test strips are inexpensive and can usually give results within 5 minutes. If you or someone you know is taking a drug, encourage them to test for fentanyl first.
In addition, pills that are marketed as opioids are not the only places this drug might be encountered. Fentanyl is being found mixed into other drugs such as cocaine and methamphetamine.12 Someone using these drugs may encounter opioids without realizing it. When a person uses substances contaminated with fentanyl, it can greatly increase their risk for overdose.
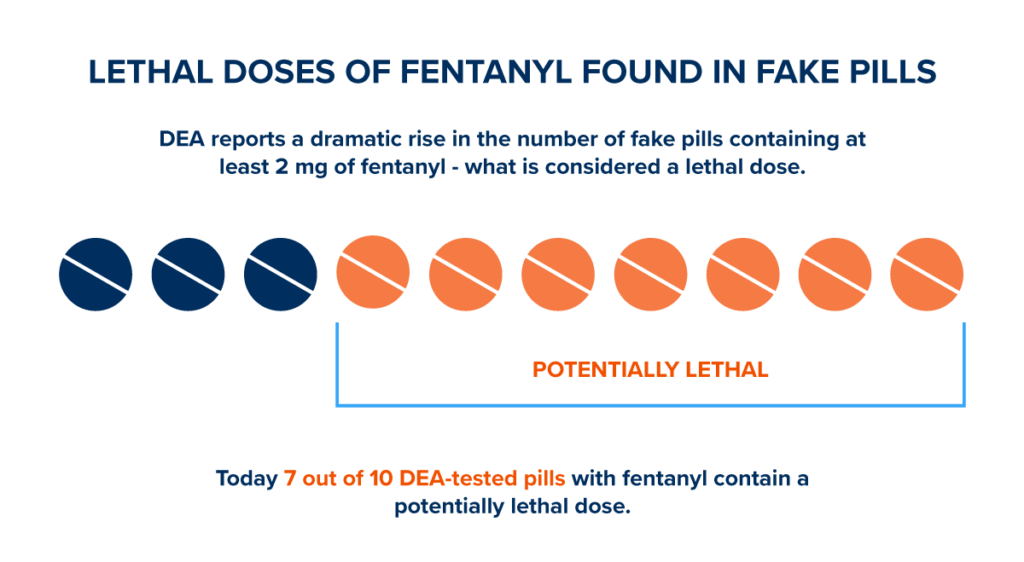
Fentanyl is much more potent than heroin or morphine. Just 2 milligrams, or 10-15 grains of table salt, is enough to be fatal.11

Learn how to use fentanyl test strips to reduce risk of an overdose.
 People who develop an addiction might act differently than they used to. They might change their friends or choose to spend a lot of time alone. They may lose interest in their favorite things, or quickly change between feeling bad and feeling good. Physical signs that someone may be misusing an opioid include drowsiness, small pupils, and slow breathing.
People who develop an addiction might act differently than they used to. They might change their friends or choose to spend a lot of time alone. They may lose interest in their favorite things, or quickly change between feeling bad and feeling good. Physical signs that someone may be misusing an opioid include drowsiness, small pupils, and slow breathing.
People with an addiction often can’t stop taking drugs on their own; you can help make sure they are able to find help. If you know someone who is using or addicted, encourage them to talk to a parent, teacher, coach, or other trusted adult. Your friend may not be ready to talk to someone about their drug use, but you can be prepared to help when they are.
The most important thing you can do is stay informed. Talk to your healthcare provider about what side effects to look for and remember to avoid stigmatizing language when urging someone to get help.
If you believe someone could use help with unsafe opioid use, consider taking the following steps:

Michigan has ten regional Prepaid Inpatient Health Plans (PIHP) to manage specialty mental health and substance use disorder treatment benefits.13 Refer to the map to find the PIHP that covers the county that the person who needs help lives in. Call the phone number listed under that PIHP for help getting connected to treatment. You may also refer to this list and call the Access phone number below your PIHP.
Community Mental Health Services in Michigan refer to a range of programs and resources provided to individuals with behavioral health challenges within their communities. These services are designed to offer support, treatment, and rehabilitation to improve an individual’s mental health and overall well-being. In Michigan, community mental health services typically include Crisis Intervention, Outpatient Services, Case Management, Psychiatric Rehabilitation, Peer Support Services, Residential Treatment, and Crisis Residential Services
 In Michigan, minors 14 years or older can access mental health services without needing the consent of a parent or guardian. This includes up to 12 sessions or four months of counseling. The resources listed below can help you or someone you know looking to access mental health services.
In Michigan, minors 14 years or older can access mental health services without needing the consent of a parent or guardian. This includes up to 12 sessions or four months of counseling. The resources listed below can help you or someone you know looking to access mental health services.
Young people might be drawn to using opioids for various reasons, similar to why adults might misuse these substances. Some of the motivations specific to adolescents include:
Teenagers are often in a stage of life characterized by curiosity and a desire to experiment with new experiences, which may include trying drugs.
Adolescents can be highly influenced by their peers. The desire to fit in or succumb to peer pressure can lead to trying opioids if they perceive them as being accepted or encouraged within their social group.
Teens may use opioids to cope with stress, anxiety, depression, or other mental health issues. They might find that opioids temporarily alleviate their problems, leading to ongoing misuse.
Some teenagers may use opioids for their euphoric effects and as a way to escape from boredom or to enhance social encounters.
Teens suffering from pain—whether physical or emotional—might use opioids to self-medicate, especially if they have access to prescription opioids from family members or friends.
The pressure to perform academically, athletically, or in other areas can sometimes lead teenagers to misuse prescription drugs, hoping to manage pain efficiently to perform better or to cope with the expectations placed on them.
Adolescents may have misconceptions about the safety of prescription drugs, thinking they are safer to use than illicit drugs.14 They might not fully understand the risks of addiction, overdose, and other health repercussions associated with opioids.
Teens may have easier access to opioids through prescriptions for themselves or family members. This can provide an opportunity for misuse that wouldn’t exist with illicit substances.
The portrayal of drug use in movies, television, music, and social media can sometimes glamorize or trivialize substance misuse, influencing teens to emulate these behaviors.
Teenagers who have experienced trauma or adverse childhood experiences (ACEs) might seek outlets for their emotional pain and find temporary solace in opioids.
When someone is experiencing an overdose, every second matters. Knowing what to do—and quickly—can help save a life and give a person another opportunity for recovery.
Naloxone is a life-saving drug that can reverse the effects of an opioid overdose. Knowing where naloxone is in your community and how to use it will ensure that you are ready to take action when in need of an emergency.
| A | Arouse: try to wake the person up |
| C | Check for overdose signs: slow or no breathing, blue/gray lips or fingernails, deep snoring/gurgling noises, unresponsive to pain, very small pupils in their eyes |
| T | Telephone 911: tell dispatch “I think it’s an overdose” and stay with the person |
| I | Intranasal Naloxone: spray Naloxone |
| O | Oxygen: do rescue breaths |
| N | Naloxone again: repeat until the person starts to wake up |
Take our Naloxone Training and learn how to take A.C.T.I.O.N to reverse an overdose.
Naloxone is a medication used to quickly reverse opioid overdose. It works by binding to the same receptors in the brain that opioids bind to, which displaces the opioids and temporarily reverses its effects. Naloxone can quickly restore normal breathing to a person whose breathing has slowed or stopped because of an opioid overdose. However, naloxone is only effective for 30 – 90 minutes, and the person who had an overdose needs immediate medical care. When they wake up, they may be irritable or have other symptoms such as body aches, diarrhea or vomiting. After the naloxone is administered, it is important to stay with the person until emergency medical help arrives, if you are comfortable doing so.
To learn more about naloxone, how to use it, and where to get it, go to: https://michigan-open.org/initiatives/naloxone/.

Dispel myths around naloxone and share resources for accessing this life-saving medication with a flyer aimed at youth audiences.

Talking about opioids and opioid use disorder can be hard. Many people hesitate to seek help for themselves or others because of the stigma surrounding addiction and overdose. Asking for help is a sign of strength, not weakness.
It’s easier to have a conversation when everyone knows what we’re talking about. Here are key facts to keep in mind:
Remember when you talk about opioids or a person with Opioid Use Disorder (OUD) to do so with respect and without using stigmatizing language. People with OUD have families, jobs, and aspirations just like you and me.

Changing our language improves outcomes for those struggling with addiction. Watch this brief video to learn more.
Opioid use disorder (OUD) is a “problematic pattern of opioid use that causes significant impairment or distress.”15 Addiction and substance use disorders (SUD) are a treatable, chronic medical disease with complex interactions between brain circuits, genetics, the environment, and an individual’s life experiences. OUD and SUD can cause people to use substances or take part in behaviors that become compulsive, despite harmful consequences. Prevention efforts and treatment approaches for OUD/SUD are generally as successful as those for other chronic diseases.16 People with OUD/SUD need the same medical care as people with diabetes or heart disease.
People with OUD experience compulsive behaviors. These compulsions are urges to behave in a certain way that you can’t resist, especially against one’s conscious wishes. Opioid use disorder affects how the brain works.17 Opioids “hijack” the brain’s reward pathways through the release of dopamine, and weaken the prefrontal cortex, which is responsible for decision-making. Using the natural processes that are used for learning, the brain preferentially focuses on and desires seeking out this substance. The capacity to respond to other sources of reward are pruned away, and the ability to make other choices is corrupted.
People with OUD have families, jobs, hobbies, and aspirations like anyone else. Adolescents and young adults have vast potential, dreams, and aspirations that extend beyond the challenges they may face with opioid use. It’s vital to see anyone experiencing substance use as individuals full of promise, capable of learning, growing, and making positive changes. By offering non-judgmental support and resources, we can help them navigate through struggles, reinforce their strengths and foster their ability to build a bright and successful future.
You may hear people laughing off taking pills or making jokes about overdose. Making jokes about people who use drugs contributes to stigma by perpetuating negative stereotypes, dehumanizing individuals, minimizing the severity of addiction, creating barriers to help-seeking, and impacting mental health. It’s important to recognize the harmful effects of such jokes and to promote empathy, understanding, and support for individuals struggling with substance use disorders.
Jokes about drug use often rely on stereotypes that portray individuals who use drugs as morally weak, irresponsible, or dangerous. These stereotypes reinforce stigmatizing attitudes and contribute to the misconception that all people who use drugs fit these negative stereotypes.
Jokes about drug use can dehumanize individuals who struggle with substance use disorders, reducing them to the butt of a joke rather than acknowledging their humanity and dignity. This dehumanization further reinforces stigma by making it easier for society to dismiss or marginalize their struggles.
Drug addiction is a complex and serious health issue, but jokes about drug use can make it seem like not a big deal or minimize its impact. This can lead to a lack of understanding about the challenges faced by individuals with substance use disorders and hinder efforts to provide them with appropriate support and treatment.
Fear of judgment can prevent individuals who use drugs from seeking help or support for their addiction. When jokes about drug use contribute to stigma, they can make it even more difficult for people to reach out for assistance, perpetuating a cycle of shame and isolation.
Hearing jokes about drug use can also have a negative impact on the mental health and well-being of individuals struggling with substance use disorders. It can increase feelings of shame, guilt, and self-stigma, making it even harder for them to seek help or engage in recovery efforts.
Talking honestly about drug use becomes easier when it is destigmatized. When people feel that they won’t be judged for discussing their experiences with drugs, it paves the way for more productive conversations about prevention, treatment, and support.
