As substance use disorders (SUD) increase across the nation, helping patients progress safely and comfortably through surgical recovery after a procedure is critical. With our SUD Care Coordination initiative, we strive to educate providers on the importance of screening for SUD and how to screen using a standardized screening tool. We also cover the basics of interpreting screening results and acting on a high-risk score. Communicating with patients about their high-risk score in a non-stigmatizing way and providing appropriate referrals to treatment or educational interventions are key to SUD care. Looking to learn more about substance use disorder? Our patient section defines SUD and substances, signs and symptoms to look out for, treatment options and locations, and support for families.

Patients with or at risk of SUD may be at higher risk for poorly controlled pain, longer lengths of stay, greater risk of complications, and greater healthcare utilization.
 | Preoperatively, as many as 2 in 5 patients may present with unhealthy substance use before elective surgery.1 |
 | Early identification presents an opportunity for further assessment, improved coordination of care, tailored pain management, and clear communication across the healthcare team. 2 |
 | Patients with any preoperative opioid use, even small amounts, are more likely to require additional opioid prescriptions after surgery. 2 |
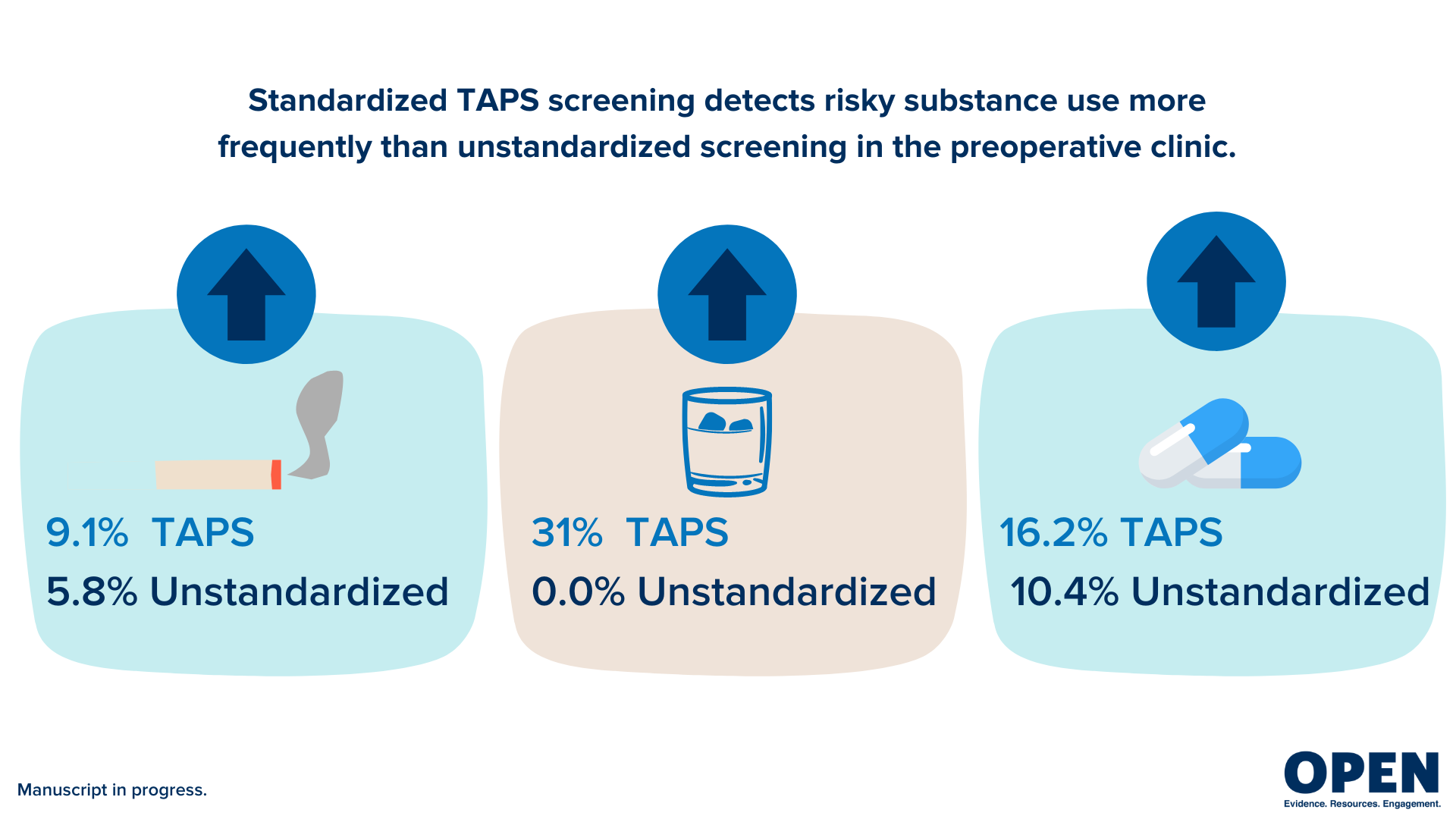
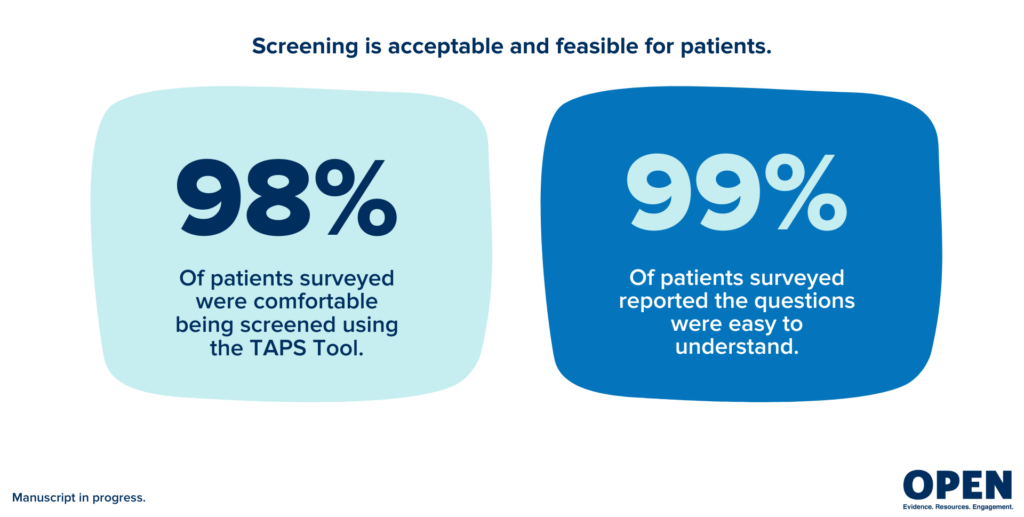
Screening is best completed using a validated, standardized screening tool such as the Tobacco, Alcohol, Prescription medications and other Substances (TAPS) questionnaire. National Institute on Drug Abuse (NIDA) provides the TAPS online for quick and easy screening as the patient or as the provider.
OPEN recommends TAPS because it is:
Patient responses to the questionnaire generate a risk score, which can help providers understand more about their patient and indicate if further assessment is needed in a non-biased way.
This free, 3-hour CE course will empower primary care providers to directly impact the opioid epidemic by learning best-practice care strategies.
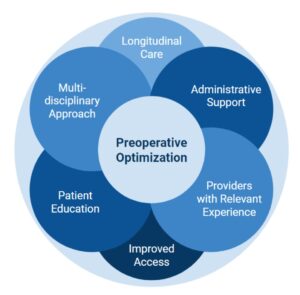
OPEN research using qualitative methods7, found that providers, including surgeons, PCPs, and anesthesiologists, value a standardized, multidisciplinary approach to perioperative opioid management focusing on:
Screening can be done by any provider caring for the patient.
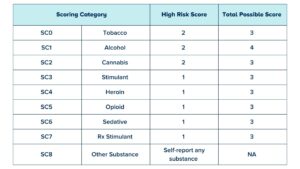
The TAPS screening is a two-part screening tool. TAPS-1 consists of 4 questions and results a positive or negative screen. If a patient screens positive, TAPS-2 substance-specific questions are activated and a risk score is calculated based on patient responses. Learn more about TAPS scoring here.8
OPEN has developed templates with recommendations for care and communication suggestions to notify a patient’s care team of positive screening results for risky substance use. For patients with positive screens for multiple categories, both categories’ resources can be cohesively combined and sent in one notification message. Prescription and non-prescription opioids have the same templates. Prescription and non-prescription stimulants have the same templates.
Learn more about how risky substance use impacts patients having surgery and best practices for identification and coordination of care for those with risky use.
A high-risk score indicates that additional assessment is needed. It is a starting point for a patient and provider conversation about substance use and how this can impact the patient’s surgical journey and long-term health outcomes.
1. CONFIRM through clinical interview and review of substance use.
2. EXPRESS CONCERN using empathy.
3. CREATE A PERIOPERATIVE PLAN proactively.
4. EDUCATE/ADVISE patient.
Having a conversation with a patient about substance use can be uncomfortable. Use the conversation starters below adapted from Empathy: Talking to Patients About Substance Use Disorder (CDC.gov).9 Additionally, check out how to use thoughtful person-centered language through OPEN’s Stigma Initiative and Shatterproof’s Addiction Language Guide.
 | ASK PERMISSION + PROVIDE OPTIONS | “Would it be ok with you if I asked you some questions about your substance use?” |
 | NORMALIZE THE CONVERSATION | “This is not unusual. Many patients find it hard to talk about their substance use.” “Talking about substance use can be uncomfortable.” |
 | BE TRANSPARENT | “I need to ask you some specific questions about your use of (substance). This will help us to determine the best plan of care for you for surgery.” |
 | ADDRESS CONFIDENTIALITY + CONCERNS HONESTLY | “I want you to know that everything you share with me and that we discuss today is confidential. However, there are some limited exceptions under the state law that I want to make sure you know and understand such as reports of threats of harm to yourself or others.” |
 | ESTABLISH TRUST AND SHOW EMPATHY | Actively listen and engage with patients in a non-judgmental way. Treat patients with respect and address their SUD as the medical disease that it is. |
 | WORK TOGETHER WITH PATIENTS | Meet patients where they are in their journey. Not every patient will be ready to stop their substance use. |
“The mission of the Center for Substance Abuse Treatment is to promote community-based substance use disorder treatment, and recovery support services for individuals and families in every community. CSAT provides national leadership to improve access, reduce barriers, and promote high-quality, life-saving, and effective treatment and recovery support services.”
“The Substance Use, Gambling and Epidemiology Section is responsible for clinical services within the Substance Use Disorder (SUD) Treatment System. Staff provide technical assistance regarding Substance Use Disorder Treatment and Recovery to Prepaid Inpatient Health Plans, providers of services, and the public. Staff are also responsible for monitoring of the system to ensure federal funding requirements are met. If you, a family member, or a friend needs treatment services for substance abuse, click above link for a local phone number to call for immediate assistance.”
If you reside in the following counties call:
“FindTreatment.gov is a product of SAMHSA’s Center for Behavioral Health Statistics and Quality (CBHSQ). It is the most comprehensive resource for persons seeking treatment for mental and substance use disorders in the United States and its territories. FindTreatment.gov provides the ability to search for substance use and mental health facilities, health care centers, buprenorphine practitioners, and opioid treatment providers.”
“Home of New Vision is a leader in the field of substance use disorder treatment and a voice in the State of Michigan. We help people find the hope, confidence, and courage to change, leading them to a new and better vision for their future. Our experience teaches us that change is possible, that treatment works, and that recovery does happen!”
“Workit Health is an online, on-demand substance use disorder treatment provider that offers medications for opioid use disorder (MOUD) via telemedicine. Workit provides treatment through mobile and web apps that keep members on track in the comfort of their own homes. Workit is in-network with commercial, Medicaid, and Medicare plans with funding available for individuals living in Washtenaw, Lenawee, Livingston, and Monroe counties who are underinsured or uninsured. Workit’s programs include provider visits, remote drug testing, 1:1 and group counseling, and online recovery courses. We offer 24/7 recovery that fits into daily life, designed by experts.”
“For many years, Dawn Farm has offered a continuum of services to help addicts and alcoholics achieve long-term recovery. With residential services, supportive transitional housing, outpatient treatment, sub-acute detoxification, and a range of active outreach programs, Dawn Farm has always been there to help.”
“Providing high-quality medication-assisted treatment to individuals aged 18 and older, Ann Arbor Comprehensive Treatment Center assists individuals who are struggling with addictions to opioids by offering the care necessary to achieve lasting recovery.”
“The WHI Opioid Project is a volunteer organization that brings together people from across Washtenaw County to end the opioid misuse and overdose epidemic in our community.”
Substance use disorder (SUD) is a complex condition that involves a problematic pattern of substance use. It can range from mild to severe (addiction). SUD is treatable just like hypertension or diabetes mellitus. It’s important to seek help as soon as possible if you think you or your child is developing SUD (Cleveland Clinic, 2022).
Substance use disorder is common. Over 20 million people in the United States have at least one SUD and affects people of all ages, races, genders and socioeconomic levels.
About 20% of people in the U.S. who have depression or an anxiety disorder also have a substance use disorder.
Of the over 20 million people in the U.S. who have SUD:
Tobacco use disorder is the most common substance use disorder worldwide and in the United States.
(Cleveland Clinic, 2022)
Substances are drugs that have addiction potential. They can be prescription drugs or non-medical drugs.
While these substances are very different from each other, they all strongly activate the reward center of your brain and produce feelings of pleasure.
These substances vary in how likely they are to lead to SUD. The likelihood is called “addiction liability,” and it depends on multiple factors, including:
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, the signs of substance use disorder include:
Seeking medical care as soon as you have signs of substance use disorder is essential.
Effective treatments are available for substance use disorder. Treatment is highly individualized — one person may need different types of treatment at different times.
Treatment for SUD often requires continuing care to be effective, as SUD is a chronic condition with the potential for both recovery and relapse.
As people with SUD often have co-occurring mental health conditions, treating them together rather than separately is generally better.
The three main forms of treatment include:
There are also several different types of treatment settings, including:
It can be very challenging and stressful to learn that someone you love may have substance use disorder. Here are some tips to help your loved one and yourself:
Families Against Narcotics (FAN) is a community-based program for those seeking recovery, those in recovery, family members affected by addiction, and community supporters.
This patient information was derived from the Cleveland Clinic website. Please visit their page for more information.
Learn more about how risky substance use impacts patients having surgery and best practices for identification and coordination of care for those with risky use.

Changing our language improves outcomes for those struggling with addiction. Watch this brief video to learn more.

This video will discuss the impact COVID-19 had on the treatment of Opioid Use Disorder.
This video details ways to manage addiction stigma while treating pain and OUD.

Explore our free financial tool to tailor insights to your organization on the potential costs and benefits of starting a transitional pain service.
Comprehensive addiction language guide to reduce use of stigmatizing language.

Emily McCall and Tim Shewcraft from the Michigan Opioid Collaborative (MOC) share information about stigma and MOC’s resources for MOUD providers. Tim, a peer recovery coach, shares his personal experience with stigma and the impacts that provider stigma can have on a patient’s OUD treatment.